Diabetic foot is a severe complication of diabetes that occurs when the nerves and blood vessels in the feet are affected.
Seemingly minor wounds can turn into hard-to-heal ulcers, infections, and, in extreme cases, lead to amputation, but early diagnosis and proper treatment can prevent these complications.
What is diabetic foot?
Diabetic foot refers to the set of neurological and vascular changes that occur in people with diabetes, which increase the risk of wounds, infections, and ulcers in the feet.
Nerve damage (neuropathy) reduces sensitivity, and poor circulation delays wound healing, which explains why even a minor cut can become a major problem.
How does diabetic foot develop in people with diabetes?
Over time, high blood sugar levels affect the nerves and blood vessels, leading to numbness, burning sensations, pain when walking, and wounds that are difficult to heal.
Against the backdrop of this neuropathy and ischemia, abnormal pressure from footwear or minor trauma can cause ulcers and deep infections of the foot.
Symptoms of Diabetic Foot.
Early recognition of diabetic foot symptoms is essential to prevent complications and amputation.
Patients may experience numbness, tingling, pain, discoloration, swelling, wounds that do not heal, or areas of very dry, cracked skin.
Neurological and circulatory signs:
- Numbness or tingling sensations, especially at night or at rest;
- Burning sensations, sharp or stabbing pains in the legs;
- Pain or weakness when walking, which improves at rest (sign of peripheral vascular disease);
- Feet that are cold to the touch or with pulses that are difficult to feel in the ankles.
Dermatological symptoms and diabetic foot ulcer:
- Open wounds or ulcers that do not heal;
- Redness, swelling, pain, or unpleasant odor around wounds;
- Calluses, corns, cracks, and very dry skin, which can become entry points for infections;
- “Hot spots” or areas that are painful to the touch, often caused by inappropriate footwear.
Prevention of diabetic foot.
Prevention is the most effective “therapy” for diabetic foot and begins with controlling blood sugar and cardiovascular risk factors.
Careful foot care, proper footwear, and regular checkups with your doctor can significantly reduce the risk of ulcers and amputations.
Blood sugar control and lifestyle:
- Maintain the best possible blood sugar control, in accordance with your diabetes specialist’s recommendations.
- Quit smoking and control your blood pressure and cholesterol to protect your blood vessels.
- Engage in appropriate physical activity, as recommended by your doctor, without overworking your feet or causing calluses.
Footwear and protection for diabetic feet:
- Wear comfortable shoes with round toes and soft soles that do not rub or squeeze your feet.
- Avoid walking barefoot, even at home, to prevent cuts or bruises.
- Check the inside of your shoes before putting them on to make sure there are no hard objects or creases in the soles.
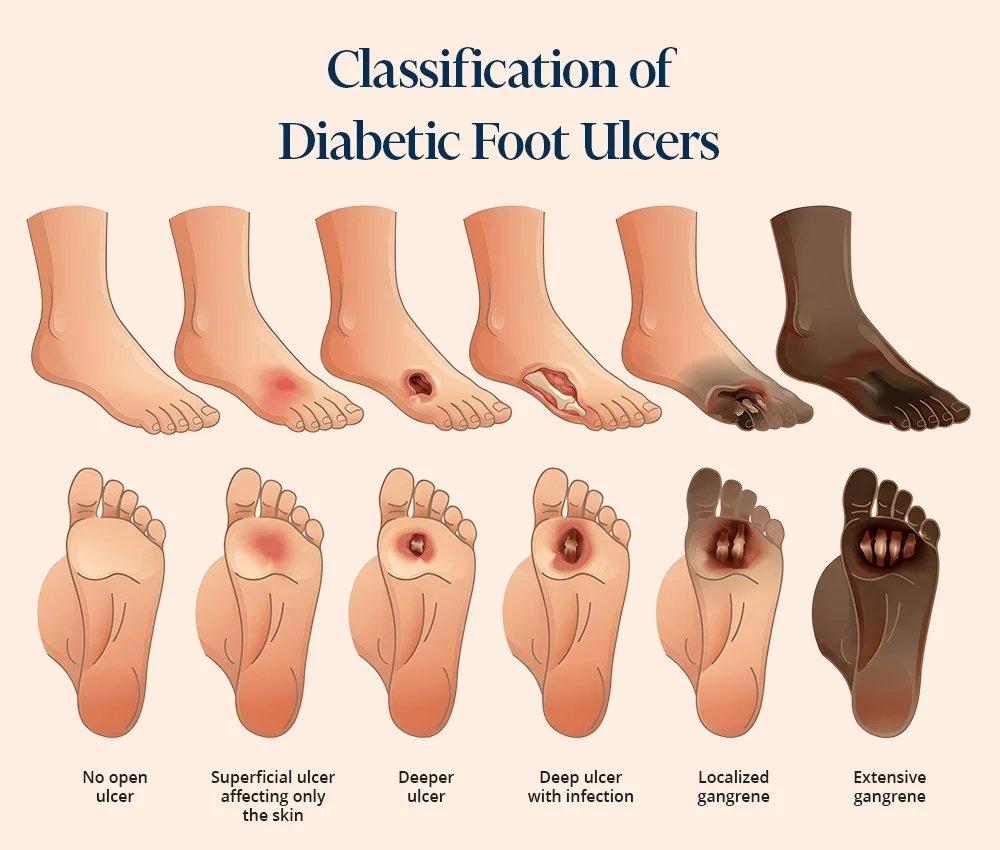
Images of diabetic foot.

Caring for diabetic feet at home.
Daily care of diabetic feet helps with early detection of wounds and prevents infections. Patients should examine their feet every day, maintain proper hygiene, and follow their doctor’s recommendations for cutting their nails and moisturizing their skin.
Daily hygiene routine:
- Wash your feet every day with warm water and soap, then dry them thoroughly, especially between the toes.
- Apply moisturizer to dry skin, avoiding the spaces between your toes to prevent excessive moisture.
- Do not put wet feet into socks and change your socks every time they get wet.
How to check your feet correctly:
- Check your skin daily for cuts, blisters, redness, swelling, or discoloration.
- Use a mirror or ask a family member to help you examine your feet and hard-to-see areas.
- Notify your doctor immediately if you notice a wound that won’t heal, pus, an unpleasant odor, or fever.



Diabetic foot treatment at the VenArt clinic
Diabetic foot treatment must be personalized, depending on the stage of the disease, the presence of ulcers, and the degree of vascular and neurological damage.
At VenArt medical clinic, the vascular surgery team uses modern approaches to heal wounds, control infections, and restore circulation in the foot, reducing the risk of amputation.
Treatment of diabetic foot ulcers:
- Professional cleaning and debridement of wounds to remove necrotic tissue and stimulate healing;
- Modern dressings adapted to the type of ulcer (dry, wet, infected) and antibiotic treatment when infection is present;
- Off-loading (pressure relief) using orthotics or special footwear to protect the affected area.
Innovative treatments and hybrid surgical procedures:
- In cases of severely impaired circulation, treatment for diabetic foot may include endovascular procedures and hybrid surgical interventions.
- At the VenArt Clinic, hybrid vascular techniques combine angioplasty with stenting and open surgery to restore blood flow to the foot and promote ulcer healing.
Read more about hybrid surgeries.
When is surgery necessary and how can we prevent amputation:
Surgery becomes necessary in cases of deep ulcers, extensive infections, severe deformities, or gangrene, when there is a vital risk or major risk to the limb.
The goal of the multidisciplinary team is to save the foot, control the infection, and restore function, with amputation being a last resort when all other options have been exhausted.
Diabetic foot complications:
Without proper treatment, diabetic foot can progress to:
- Infections;
- Foot deformities;
- Diabetic gangrene;
- Diabetic foot amputation.
Ignoring symptoms or using improvised treatments, including natural remedies without medical advice, significantly increases the risk of complications.
Neuropathic osteoarthropathy (Charcot foot)
Charcot neuropathy occurs when diabetic neuropathy causes the bones and joints of the foot to weaken, leading to microfractures and progressive deformities.
The foot can become visibly deformed, which increases local pressure and the risk of developing ulcers that are difficult to treat.
Treatment for Osteoarthropathy
In the early stages, immobilization in a cast or special orthotics helps stabilize the foot and prevent fractures and deformities.
In advanced cases, with fractured bones or dislocated joints, surgical correction may be necessary to realign the bone structure and restore stability to the foot.
When should you seek emergency medical attention?
It is essential to see a doctor urgently if there are signs of infection or vascular compromise.
Do not delay seeking medical advice if you notice: a worsening wound, extensive redness, purulent discharge, fever, chills, or severe color changes (very pale, purple, or black foot).
Frequently asked questions about diabetic foot.
Diabetic foot is a complication of diabetes in which the nerves and blood vessels in the feet are affected, increasing the risk of wounds and infections.
It usually occurs after years of diabetes with inadequate glycemic control and is exacerbated by smoking, hypertension, high cholesterol, and inappropriate footwear.
Early signs include numbness, tingling, burning, cold feet, pain when walking, and very dry or cracked skin.
Later, small wounds that do not heal, painful calluses, discoloration, or persistent swelling may occur.
Treatment combines local wound care, infection control, protection of the affected area and, when necessary, procedures to improve blood circulation.
In the VenArt clinic, the vascular surgeon decides on the treatment plan, which may include debridement, modern dressings, antibiotics and hybrid vascular interventions, to save the leg.
Untreated, the diabetic foot can progress to serious infections, osteomyelitis (bone infection), gangrene, and ultimately amputation.
In addition, the presence of severe ulcers and infections increases the risk of hospitalization and significantly affects quality of life.
Yes, controlling blood sugar, quitting smoking, wearing appropriate footwear, and examining your feet daily significantly reduce the risk of ulcers. Regular consultations with a diabetologist and vascular surgeon help identify problems early and prevent complications.
Comfortable shoes with a wide toe, soft soles and no internal seams that rub the skin are recommended.
In some cases, the doctor may recommend orthopedic shoes or custom orthotics to reduce local pressures and protect vulnerable areas.
See a doctor immediately if you notice a spreading wound, signs of infection (redness, local warmth, pus, unpleasant odor), fever, or chills. Also, see a doctor immediately if your leg becomes very pale, purple, or black, or if pain when walking suddenly worsens.
Schedule a consultation at the VenArt Clinic.
If you have diabetes and have noticed changes in your feet, don’t wait for the symptoms to get worse.
Schedule a consultation at the VenArt clinic in Cluj or Bucharest for a diabetic foot evaluation and a personalized treatment plan, adapted to the stage of the disease and your needs.
For more information, do not hesitate to contact us.
Updates and Resources.
We provide the latest information on diabetic foot care, prevention and innovative treatments to combat complications such as diabetic ulcers and neuropathy. Supporting the diabetic community in effectively managing this condition. By constantly updating content and providing valuable resources, we aspire to be a trusted support in maintaining a healthy life.
Yap, Moi Hoon, et al. “A New Mobile Application for Standardizing Diabetic Foot Images.” Journal of Diabetes Science and Technology, vol. 12, no. 1, 21 June 2017, pp. 169–173, https://pubmed.ncbi.nlm.nih.gov, 10.1177/1932296817713761
Interactive calculator to estimate insulin sensitivity in type 1 diabetes https://pubmed.ncbi.nlm.nih.gov/38366869/ Januszewski AS, Niedzwiecki P, Sachithanandan N, Ward GM, O’Neal DN, Zozulinska-Ziolkiewicz DA, Uruska AA, Jenkins AJ. J Diabetes Investig. 2024 Feb 17. doi: 10.1111/jdi.14161.
Conclusion.
The diabetic foot should not be underestimated, and a proactive attitude can make the difference in preventing severe complications. Prevention and care of the diabetic foot requires close collaboration with the medical team, so that any problems are identified and treated in the early stages. Constant monitoring, proper care and regular consultation with the doctor can help maintain foot health and avoid more serious problems associated with this condition.
It is essential to seek medical attention when you notice any change in the color of the skin on your feet or other symptoms related to the diabetic foot.
Medical consultant: Prof. Dr. Jérôme Cau











