Technological advances in recent years have greatly improved the accurate diagnosis of post-thrombotic vascular disorders. Some of these conditions are rare but can now be treated using modern minimally invasive techniques. Conditions caused by venous compression, such as May-Thurner and Nutcracker syndromes, where the affected vein is compressed, can lead to a range of uncomfortable and sometimes severe symptoms. Recently, venous stenting has emerged as an innovative treatment, offering new hope and relief for patients living with these conditions.
Understanding Post-Thrombotic Syndrome
Post-thrombotic syndrome is a long-term complication of deep vein thrombosis (DVT), which is when blood clots form in the deep veins, most commonly in the legs or pelvis. PTS develops in up to 50% of individuals who have experienced DVT and can significantly impact daily activities due to chronic pain, swelling, and, in severe cases, venous ulcers.
The Role Of Venous Stenting In PTS
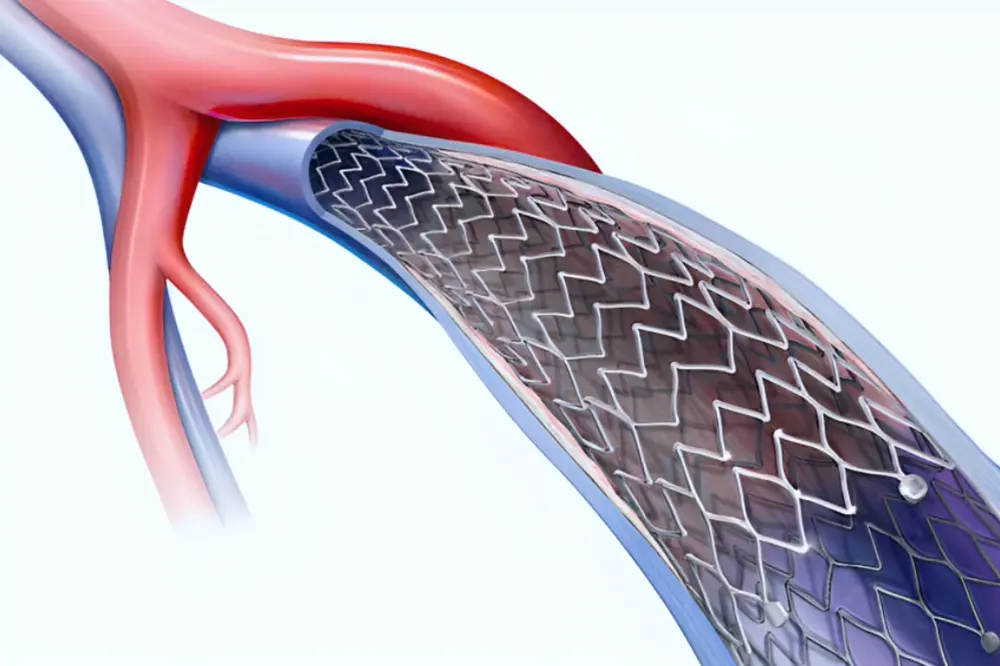
Venous stenting has become increasingly important in the treatment of PTS, especially in cases involving the pelvic veins. This minimally invasive procedure involves placing a stent—a small, mesh-like tube—inside the affected vein to keep it open and improve blood flow.
Benefits Of Venous Stenting For PTS For The Pelvic Vein
- Symptom Relief: Venous stenting can greatly reduce symptoms related to PTS, including pain, swelling, and skin changes.
- Minimally Invasive: Compared to traditional surgical options, venous stenting is less invasive, which helps patients recover faster with less discomfort.
- Improved Quality Of Life: Many patients report significant improvements in daily comfort and mobility after treatment.
- Reduced Risk Of Recurrence: Stenting helps prevent new blood clots from forming in the treated area, providing long-term benefits.
The Procedure: What To Expect
During the venous stenting procedure, a small incision is usually made in the groin area. Using imaging guidance, a catheter is carefully directed to the affected vein. The stent is then placed to keep the vein open and restore normal blood flow. The procedure typically lasts between one and two hours and is often performed under local anesthesia.
Ideal Candidates For Venous Stenting
Not all patients with PTS are suitable candidates for venous stenting. Ideal candidates generally have:
- Chronic symptoms that do not improve with conservative treatments.
- Clear evidence of a blockage or significant narrowing of the veins based on imaging studies.
- Good overall health to safely undergo the procedure.
Post-Procedure Care And Monitoring
After venous stenting, patients will follow a specific medication plan, including anticoagulants, to help prevent new clots from forming. Regular follow-up appointments are essential to monitor the stent and the overall health of the veins.
Risks And Considerations
As with any medical procedure, venous stenting carries some risks, including bleeding, infection, and the possibility of blood clots. It is important to discuss all potential risks and benefits with your healthcare provider.
Conclusion
Venous stenting for pelvic PTS represents a major step forward in treating this challenging condition. By offering a minimally invasive solution with long-term benefits, this technique has transformed how post-thrombotic syndrome is managed, giving patients new hope and a better quality of life.
For more information or to schedule a consultation, please contact us here.