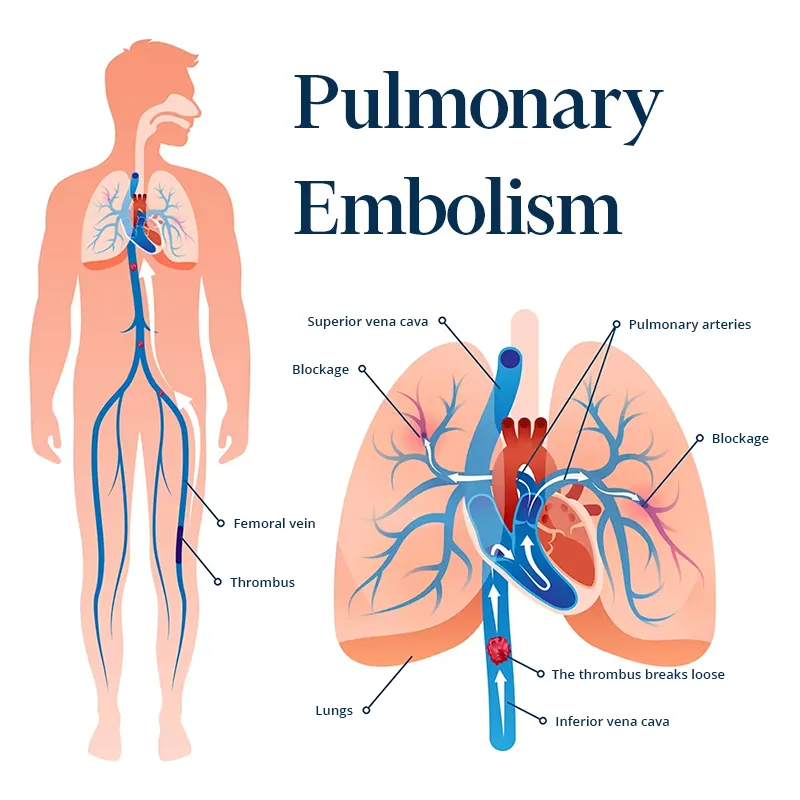
What Is Pulmonary Embolism?
Pulmonary embolism is a life-threatening condition that occurs when a blood clot blocks one or more arteries in the lungs. In most cases, these clots form in the deep veins of the legs or pelvis, a condition known as deep vein thrombosis, and then travel through the bloodstream to the lungs.
Causes And Risk Factors
The most frequent cause of pulmonary embolism is deep vein thrombosis. Certain factors increase the risk of developing pulmonary embolism, including:
- Prolonged immobilization (hospital stays, long-distance flights, or extended bed rest);
- Recent surgery, especially orthopedic or abdominal operations;
- Pregnancy and the postpartum period;
- Use of oral contraceptives or hormone replacement therapy;
- Smoking;
- Obesity;
- Personal or family history of blood clots;
- Cancer;
- Advanced age;
- Chronic heart or lung disease.
Common Symptoms
Pulmonary embolism can present with no symptoms, mild discomfort, or severe manifestations. The most common signs and symptoms include:
- Sudden shortness of breath (dyspnea);
- Chest pain that worsens when breathing deeply;
- Cough, which may produce blood (hemoptysis);
- Rapid heartbeat (tachycardia);
- Lightheadedness, dizziness, or fainting;
- Sudden onset of anxiety or restlessness;
- Pale or bluish skin (cyanosis).
Possible Complications
Without timely treatment, pulmonary embolism can be fatal. Potential complications include:
- Chronic pulmonary hypertension – persistent high blood pressure in the lung arteries;
- Right-sided heart failure;
- Sudden death in severe cases;
- Recurrence – increased risk of another embolism without proper long-term management.
Diagnosis
To confirm pulmonary embolism, the doctor may order several tests, such as:
- Blood tests (D-dimer levels);
- CT pulmonary angiography with contrast, which visualizes blood flow in the lungs;
- Doppler ultrasound of the legs to detect deep vein thrombosis;
- Pulmonary scintigraphy, used in selected cases;
- Electrocardiogram (ECG) and chest X-ray to rule out other conditions with similar symptoms.
Treatment
The choice of treatment depends on the severity of the embolism and the overall health of the patient.
Anticoagulants
- Medications that prevent new clots from forming and stop existing clots from growing. Examples include heparin, warfarin, rivaroxaban, and apixaban.
- The duration of treatment varies and may last from three months to lifelong therapy, depending on individual risk factors.
Thrombolytics
- Drugs designed to dissolve clots rapidly;
- These are reserved for severe cases due to the increased risk of bleeding.
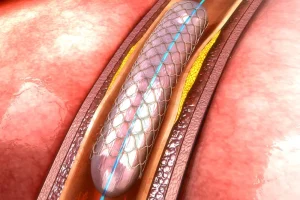
Inferior Vena Cava Filter
- A device inserted into the inferior vena cava to stop clots from reaching the lungs;
- Used in patients who cannot receive anticoagulant treatment.
Oxygen Therapy And Respiratory Support
- Oxygen is provided in cases of breathing difficulty or low blood oxygen levels;
- In severe cases, additional respiratory support may be required.
Recovery And Lifestyle After Pulmonary Embolism
Recovery involves both medical treatment and lifestyle adjustments to prevent recurrence. Patients are advised to:
- Follow medical prescriptions and take anticoagulant medication as directed;
- Avoid prolonged periods of immobility, especially during travel;
- Stop smoking completely;
- Maintain a healthy body weight;
- Drink sufficient fluids daily to avoid dehydration;
- Wear compression stockings if recommended by the doctor;
- Engage in regular physical activity appropriate to their condition.
Conclusion
Pulmonary embolism is a medical emergency that requires immediate diagnosis and treatment. With proper therapy, most patients recover well and return to their normal activities. Long-term prevention through lifestyle modifications and adherence to medical advice is crucial to reducing the risk of complications and recurrence. Schedule an appointment with us and see how we can help.