Women of reproductive age often develop uterine fibroids, which are non-cancerous growths that form in the walls of the uterus. Their size can range from microscopic, invisible to the human eye, to large growths that distort and enlarge the uterus. These fibroids are not linked to an increased risk of uterine cancer. In very rare cases, they may become cancerous.
Uterine Fibroids – Symptoms
In most cases, uterine fibroids, especially those that remain small, do not cause noticeable symptoms. This is why annual gynecological check-ups are essential, allowing doctors to detect abnormalities early and recommend monitoring or treatment.
When symptoms do occur, they vary based on the size, number, and location of the fibroids. Women should be aware that fibroids can impact their daily life and reproductive health.
For women who do experience symptoms, the most common include heavy menstrual bleeding and prolonged menstrual periods lasting more than seven days. Other symptoms may involve pelvic pressure, pelvic pain, and frequent urination.
Some women also report difficulty urinating, constipation, or lower back and leg pain. In rare cases, acute pain occurs when the blood supply to a fibroid is disrupted and the fibroid begins to die.
What Causes Uterine Fibroids?
The exact cause of uterine fibroids remains unknown, although several contributing factors have been identified.
Hormonal influences are believed to play a major role, as fibroids contain more estrogen and progesterone receptors than normal uterine tissue. This explains why fibroids tend to shrink after menopause when hormone production naturally declines. Research has also revealed that fibroid cells often display genetic differences compared to normal uterine muscle cells.
Other factors have also been implicated in fibroid growth. Growth-promoting substances in the body, such as insulin-like growth factor, may encourage their development.
In addition, fibroids typically contain excessive amounts of extracellular matrix, which is the material that supports and connects cells. This accumulation contributes both to fibroid size and to structural changes in the uterus.
Uterine Fibroids – Treatment
Fibroids are often discovered during routine checkups when irregularities in the uterus are detected. Because they are non-cancerous and often grow slowly or not at all, many women with mild or no symptoms may choose not to pursue treatment. Fibroids also tend to shrink naturally after menopause due to decreased hormone production. However, ongoing monitoring is always recommended to track their progression.
When symptoms are mild, doctors may suggest medication to relieve pain and reduce heavy bleeding. Over-the-counter options such as ibuprofen or paracetamol are commonly recommended.
For women experiencing significant blood loss, iron supplements may help prevent anemia. These conservative approaches aim to control symptoms without resorting immediately to surgical interventions.
Hormonal treatments are among the most widely used methods for managing fibroids. Low-dose contraceptives, progesterone injections, and intrauterine devices such as Mirena can regulate menstruation, reduce heavy bleeding, and stop fibroid growth.
Gonadotropin-releasing hormone agonists are also prescribed to shrink fibroids temporarily, especially before surgery. Although they can cause side effects like hot flashes, joint pain, or decreased libido, most women tolerate them well.
If symptoms are moderate to severe and conservative measures fail, surgical treatment may be necessary. The most common surgical procedures include myomectomy, hysterectomy, endometrial ablation, myolysis, and uterine fibroid embolization. Each method is selected based on the severity of symptoms, patient preference, and fertility considerations. Consultation with a specialist is critical to choose the most appropriate option.
Uterine Fibroids – Surgery
- Myomectomy: Removal of fibroids while preserving healthy uterine tissue, recommended for women wishing to maintain fertility.
- Hysterectomy: Complete removal of the uterus, considered for severe cases or when fertility is not a concern;
- Endometrial Ablation: Removal or destruction of the uterine lining to reduce heavy bleeding;
- Myolysis: Use of laparoscopy-guided needles with electricity or freezing to destroy fibroids;
- Uterine Fibroid Embolization: Blocking the blood supply to fibroids, causing them to shrink over time.
At VenArt Clinic, specialists in gynecological surgery and gynecological oncology apply advanced surgical techniques to ensure optimal results. Our experienced surgeons deliver safe and effective treatment tailored to each patient’s unique condition. Innovative medical technology further enhances the precision of these procedures. Patients benefit from both long-term results and improved quality of life. For more details, check our gynecological oncology section. You can also schedule a consultation with our clinic to see how we can help.
Do Uterine Fibroids Affect Female Fertility?
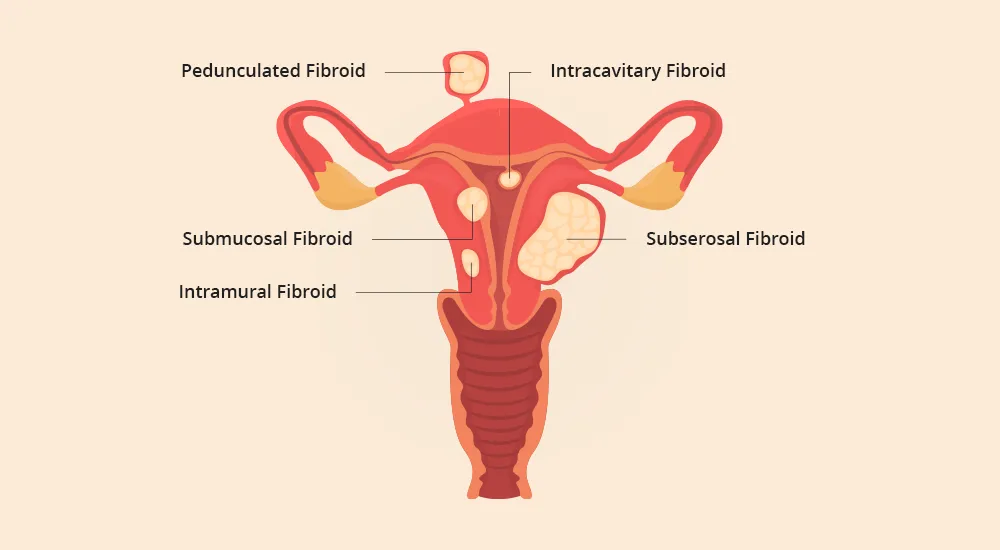
The impact of fibroids on fertility depends on their size and location. Large fibroids inside the uterine cavity may interfere with conception and pregnancy. However, fibroids that develop on the outer surface of the uterus and remain small usually do not affect fertility. In some cases, hormonal changes during pregnancy can even reduce fibroid size.
Uterine Fibroids During Pregnancy
Fibroids may complicate pregnancy in certain cases, particularly when they distort the uterine cavity. Their growth can influence implantation, fetal development, or lead to pregnancy-related discomfort. Careful monitoring during pregnancy is important to manage these risks. Fortunately, many women with fibroids experience healthy pregnancies.
Uterine Fibroids And Sex Life
Several theories explain how fibroids may contribute to infertility or sexual difficulties. Changes in the cervix may reduce the number of sperm reaching the egg, while uterine shape changes can hinder sperm movement or embryo implantation. Fibroids may also block the fallopian tubes or affect the uterine lining. Additionally, reduced blood supply may prevent successful embryo implantation.











