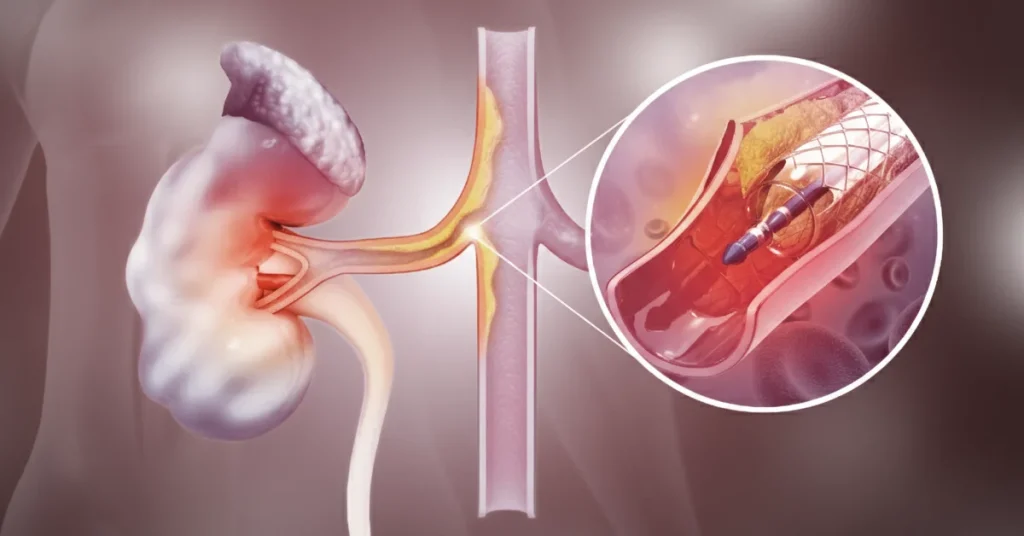
Angioplasty and stenting of the renal arteries are minimally invasive procedures used to treat renal artery stenosis, the narrowing of the blood vessels that carry blood to the kidneys, with the goal of improving blood pressure control and protecting kidney function.
Many patients know this intervention as a “kidney stent,” especially when they have hard-to-control hypertension or worsening kidney failure.
What is Renal Artery Stenosis?
Renal artery stenosis means narrowing of one or both arteries that supply blood to the kidneys, usually due to the deposition of fat and calcium (atherosclerosis) on the vessel walls.
This “narrowing of the renal artery” reduces blood flow to the kidneys and can cause renovascular hypertension (kidney-related high blood pressure), which is difficult to control with medication, as well as progressive deterioration of kidney function.
Common Causes of Renal Artery Stenosis
- Atherosclerosis of the renal artery: cholesterol and calcium plaques that narrow the vessel lumen; it is the most common cause in older patients with cardiovascular risk factors (smoking, diabetes, high cholesterol, hypertension).
- Fibromuscular dysplasia: non-atherosclerotic involvement of the arterial wall, more common in younger people, especially women, with narrowing of the renal arteries.
- Rare causes: vasculitis, trauma, or external compression (tumors, anatomical anomalies).
Symptoms and Warning Signs in Renal Artery Stenosis
Often, renal artery stenosis does not cause specific symptoms and is discovered incidentally on ultrasound or CT angiography. However, there are situations that should raise suspicion of renovascular hypertension and prompt referral to a specialist:
- Sudden onset of arterial hypertension in an adult over 50 years old or very difficult-to-control blood pressure, despite treatment with several antihypertensive drugs.
- Sudden rise in creatinine and decrease in glomerular filtration rate, especially after starting certain antihypertensive drugs (renin–angiotensin system blockers).
- Episodes of acute heart failure or “flash” pulmonary edema in a patient with very high blood pressure and suspected renovascular disease.
How is Renal Artery Stenosis Diagnosed?
The diagnosis of renal artery stenosis combines clinical examination with imaging investigations of the renal arteries.
Renal Artery Doppler Ultrasound
- Renal artery Doppler ultrasound is usually the first recommended test for “narrowing of the kidney vessels”. It allows assessment of the renal artery lumen and blood flow velocities, providing clues about stenosis severity.
CT Angiography or MR Angiography of the Renal Arteries
- CT angiography of the renal arteries and MR angiography are non-invasive tests that show renal artery anatomy, stenosis location and length, and the condition of the aorta and other vessels.
Renal Arteriography (Selective Angiography)
- Renal arteriography is an invasive angiography that visualizes the renal artery directly. Its major advantage is that, in the same session, if a significant stenosis is confirmed, balloon angioplasty and stent implantation in the renal artery can be performed.
In addition to these investigations, the physician monitors the blood pressure profile, creatinine trend, kidney size, and overall cardiovascular context.
When is Stent Angioplasty Indicated for Renal Artery Stenosis?
Not all renal artery stenoses require renal artery surgery or a minimally invasive procedure; many cases can be treated with medication and monitoring alone. Renal angioplasty with stent is reserved for patients in whom stenosis has important clinical consequences and there is a real chance to improve blood pressure and kidney function.
Typical Situations Where Renal Artery Stenting is Considered
- Accelerated or treatment-resistant hypertension associated with significant renal artery stenosis.
- Worsening kidney function (elevated creatinine, reduced GFR) in the context of hemodynamically significant stenosis.
- Recurrent episodes of heart failure or acute pulmonary edema (“flash pulmonary edema”) in patients with bilateral renal artery stenosis or a solitary functioning kidney.
- Selected situations where protection of a still viable kidney with severe stenosis is desired, before permanent loss of function.
The decision to stent the renal artery is usually made by a multidisciplinary team (vascular and endovascular surgery, cardiology) to correctly evaluate the benefit/risk ratio.
What are Renal Angioplasty and Stenting?
Renal artery angioplasty is a minimally invasive procedure in which a balloon is advanced to the narrowed segment and inflated to widen the arterial lumen. Renal artery stenting involves placing a small metal tube (stent) at the stenosis site to keep the vessel open long term and reduce the risk of re-narrowing (restenosis).
Types of Stents Used in Renal Angioplasty with Stent
- Bare-metal stents: classic stents with a restenosis risk around 10–20% in some series, especially in small-caliber arteries.
- Drug-eluting stents: coated with antiproliferative drugs, which significantly reduce restenosis risk in some patients.
Renal Angioplasty with Stent: Step-by-Step Procedure
The renal angioplasty with stent placement procedure is performed in an angiography suite, under fluoroscopic guidance, usually with local anesthesia and mild sedation.
1. Patient Preparation
- Detailed clinical and laboratory evaluation, and possible adjustment of treatments (anticoagulants, antidiabetics, diuretics).
- Adequate hydration and measures to protect kidney function, considering the use of contrast agent (prevention of contrast nephropathy).
2. Vascular Access
- Arterial puncture in the groin (femoral artery) or, in some cases, radial access at the wrist.
- Introduction of an arterial sheath through which catheters are advanced to the renal arteries under X-ray guidance.
3. Diagnostic Angiography
- Injection of contrast medium to precisely visualize the stenosis, measure the renal artery diameter and length, and plan balloon dilation and stenting.
4. Balloon Angioplasty
- Positioning the balloon at the narrowed segment and inflating it for several tens of seconds to widen the arterial lumen.
5. Renal Stent Implantation
- If balloon angioplasty alone is insufficient or the lesion is complex, a metal stent is implanted in the renal artery, which remains fixed in the vessel wall and keeps the artery open.
6. Hemostasis at the Puncture Site
- After completing the procedure, catheters and sheaths are removed, and manual compression or an arterial closure device is applied at the puncture site, followed by a pressure dressing.
In general, a renal artery angioplasty lasts between 30 and 60 minutes, depending on anatomy and the number of lesions treated.
Kidney Stent for Renovascular Hypertension
For many patients, the main question is: “Will a kidney stent help my blood pressure?” In correctly selected patients, treatment of renal artery stenosis by angioplasty and stent can:
- Lower blood pressure values and/or reduce the number of required medications.
- Stabilize or improve kidney function.
- Reduce episodes of heart failure or acute pulmonary edema.
However, the procedure is not indicated for all patients with high blood pressure; in many cases, medical treatment of renal stenosis remains the first-line option according to European guidelines.
Recovery After Renal Angioplasty with Stent
Most patients stay in the hospital for about 24 hours for observation, blood pressure control, and kidney function monitoring. Light activities can be resumed within a few days, avoiding intense exertion and heavy lifting during the first week to protect the puncture site.
Treatment and Follow-up After the Procedure
- Antiplatelet medications (e.g., aspirin ± another antiplatelet) to prevent stent thrombosis and restenosis.
- Adjustment of antihypertensive therapy according to the new blood pressure values, which may improve significantly after revascularization.
- Periodic monitoring of kidney function and, when needed, imaging follow-up (renal artery Doppler ultrasound, CT angiography) to check stent patency.
Benefits and Limits of Renal Artery Stenting
The main goals of renal artery angioplasty with stent are:
- Better blood pressure control (especially in renovascular hypertension).
- Protection or stabilization of kidney function in patients with severe renal artery stenosis.
Benefits May Include
- Lower blood pressure values and/or reduction in the number of medications.
- Stabilization or sometimes improvement of kidney function if the kidney is still viable.
- Reduced frequency of heart failure episodes and acute pulmonary edema in certain patients.
Important to Understand
- The procedure is not recommended for all cases of renal artery stenosis; in some situations, the best option is medical treatment alone.
- Blood pressure and kidney response vary from patient to patient, depending on lesion duration and severity, comorbidities, and whether one or both kidneys are affected.
Risks and Possible Complications of Renal Angioplasty
Like any invasive procedure, renal artery angioplasty and stenting carry certain risks, although in experienced centers they are generally rare.
Possible Complications Include
- Allergic reactions to contrast agent or to medications used.
- Complications at the puncture site: bleeding, hematoma, rarely arteriovenous fistulas or pseudoaneurysms.
- Temporary worsening of kidney function or, rarely, acute kidney failure, especially in patients with pre-existing kidney disease (such as contrast nephropathy).
- Local vascular complications: arterial wall dissection, vessel rupture, or embolization of atherosclerotic debris.
- Rare systemic events: stroke, lower limb ischemia, or severe renal ischemia.
In specialized centers, the medical team carefully evaluates the benefit/risk ratio and is prepared to prevent or promptly manage most complications.
Why Choose VenArt Clinic for Renal Artery Angioplasty and Stenting
VenArt Clinic offers treatment for renal artery stenosis in a vascular and endovascular surgery center with experience in renal artery angioplasty and complex revascularization procedures using minimally invasive techniques. Patients benefit from:
- An international multidisciplinary team (vascular and endovascular surgery, cardiology).
- Modern imaging and angiography technology.
- Treatment protocols aligned with the latest European recommendations for renovascular hypertension and renovascular disease.
If you have been diagnosed with renal artery stenosis, have hard-to-control hypertension, or elevated creatinine values, you can discuss with a VenArt Clinic specialist about treatment options, including renal angioplasty with stent, a minimally invasive procedure designed to protect the kidneys and improve quality of life.
Frequently Asked Questions
In the absence of complications, the hospital stay is usually around 24 hours, to monitor blood pressure, heart rate, urine output and kidney function.
Light activities can be resumed after a few days, but you should avoid heavy lifting and intense physical effort during the first week to protect the puncture site.
Full recovery and stabilisation of blood pressure are assessed over time at follow‑up appointments.
Your doctor will explain exactly how your medication will be adjusted, which tests are needed and when you should come to the clinic.
Sometimes, to protect the kidneys, extra hydration is recommended and certain medicines may need to be stopped temporarily before the procedure.
Renal artery angioplasty and stenting are recommended only in selected cases of renal artery stenosis, when the narrowing of the vessel causes serious problems such as hard‑to‑control high blood pressure, worsening kidney function or episodes of heart failure and acute pulmonary oedema.
If medication alone is not sufficient, your doctor may suggest renal artery angioplasty as a minimally invasive treatment for renal artery stenosis.
The decision is made individually, after investigations (Doppler ultrasound, CT angiography/arteriography) and discussion within a multidisciplinary team.
In many cases, renal artery stenosis is initially treated with medication: strict control of blood pressure, cholesterol and cardiovascular risk factors.
Renal artery angioplasty with stent is a minimally invasive treatment reserved for patients in whom the narrowing of the artery leads to resistant hypertension, declining kidney function or episodes of heart failure.
The choice between “medication only” and revascularisation by angioplasty and stenting is made on a case‑by‑case basis, based on imaging results and current guideline recommendations.
In some patients, the number and doses of blood pressure medicines can be reduced after successful renal artery angioplasty with stent, but treatment is often still needed, adjusted to the new clinical situation.
Yes, the stent remains permanently in the artery and becomes integrated into the vessel wall, helping to keep the artery open over the long term.
Over time, there is a risk of restenosis (re‑narrowing), but this risk can be lower when drug‑eluting stents are used.