In this case study, we present a patient with an abdominal aortic aneurysm and a large aneurysm of the left iliac artery, treated using the endovascular EVAR procedure – a minimally invasive alternative to classic open surgery, with small incisions, lower risk of complications and faster recovery.
Patient situation and diagnosis
The patient had a dilatation (aneurysm) of the main blood vessel in the abdomen (the aorta), measuring approximately 3–3.5 cm, as well as a large aneurysm (over 5 cm) on one of its major branches, the left iliac artery. Aneurysms are like “ticking time bombs”: the arterial wall becomes thinner, and there is a risk that, at some point, it will rupture, leading to massive internal bleeding and, very often, death if treatment is not provided immediately.
The patient also had other vascular problems and was not a good candidate for conventional open surgery, which requires opening the abdomen and general anaesthesia. Therefore, the team chose a less invasive solution, using local anaesthesia and small incisions in the groins: endovascular aneurysm repair (EVAR).
How the EVAR procedure is performed, step by step
- The vascular surgeon inserts thin tubes and guidewires through the arteries in the groins (the femoral arteries), without opening the abdomen.
- Inside the dilated vessel (the aneurysm), a special “prosthesis” (stent graft) made of fabric on a metal frame is advanced and then deployed in the diseased segment.
- This stent graft redirects the blood flow through its inner lumen, so that the pressure no longer acts on the weakened aneurysm wall; in practical terms, the aneurysm is “excluded” from direct circulation and the risk of rupture drops significantly.
In this particular case:
- The medical team first closed one branch (the left hypogastric/internal iliac artery) with a vascular plug, to prevent complications and backflow of blood into the aneurysm sac.
- Then the main body of the stent graft was positioned just below the renal arteries, with two “limbs” extending into the left and right iliac arteries, so that blood could flow properly to both legs.
- For the right limb of the stent graft, an additional access through the artery in the arm was required in order to successfully catheterise the vessel – a more complex technique, but commonly used in experienced centres.
Immediate result after treatment
At the end of the procedure, angiographic control with contrast showed that:
- There was no leakage of blood around the stent graft (no “endoleak”).
- The aneurysm was completely excluded from the circulation.
- The stent graft was fully open and functioning well in both limbs.
The patient was stable, with proper closure of the puncture sites and a clear plan for medication (aspirin, anticoagulant therapy) and regular imaging follow-up.
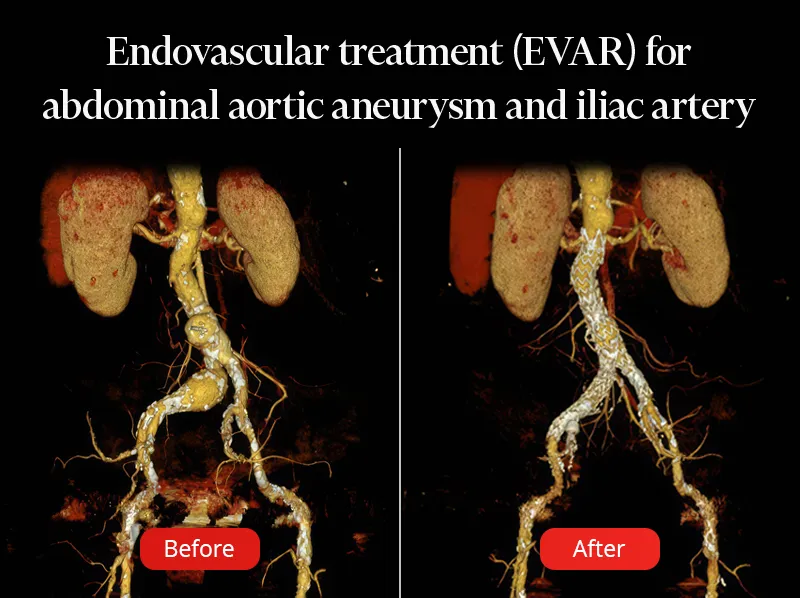
Before the EVAR procedure, the two aneurysms (bulges) that were putting the patient’s life at risk can be clearly seen.
In the image on the right, you can see the repaired area with the stent graft in place, and the risk of rupture of these major arteries has been eliminated.
What patients should know about aneurysms and EVAR
What is an aortic aneurysm and what are the risks?
- An aneurysm is a “bulge” in an artery: the vessel wall stretches and becomes thinner, like an overinflated balloon.
- The larger the diameter, the higher the risk that this “balloon” will burst (rupture). In the case of the aorta, this can lead within minutes to collapse and death, even if the ambulance arrives quickly.
If a patient knows they have an aneurysm but delays or refuses the recommended treatment:
- They live with a constant risk of rupture, especially if the aneurysm is large or growing quickly.
- Ruptured aortic aneurysms carry a very high mortality rate; many patients do not even reach the operating theatre.
Why is endovascular treatment (EVAR) useful?
In the case described here:
- The patient was not suited for classic open surgery with general anaesthesia, but EVAR made it possible to repair the aneurysm under local anaesthesia with small incisions.
- Hospital stay is usually shorter, postoperative pain is reduced, and recovery is faster compared with open surgery.
For the patient, this means:
- A major reduction in the risk of aneurysm rupture.
- A lower risk of severe complications or death related to the aneurysm.
- The possibility of returning to a relatively normal life, with periodic follow-up.
Why is it not enough to “just keep watching” forever?
- Small aneurysms can be monitored, but once they reach a certain size or start to grow, the risk of rupture becomes too high, and the benefit of intervention outweighs the risks.
- Ignoring medical advice (for example, “I’ll wait another year, it doesn’t hurt”) can lead to emergency situations in which the chances of survival are much lower than with a planned procedure.
Key message for patients
- Large aortic aneurysms do not always cause pain, but they can be life-threatening if they rupture.
- When a doctor recommends an intervention (open surgery or EVAR), it is because the risk of rupture is higher than the risk of the operation itself.
- Endovascular treatment, as in this case, can offer a safe and less invasive solution, especially for frail patients or those with multiple other conditions.
- After treatment, medication (aspirin and, where appropriate, anticoagulants) and regular imaging tests (such as CT angiography) are essential to check the stent graft and prevent complications.
On the CT scan performed one month after the procedure, the result is excellent, with no signs of complications or endoleak.








