Conditions Treated
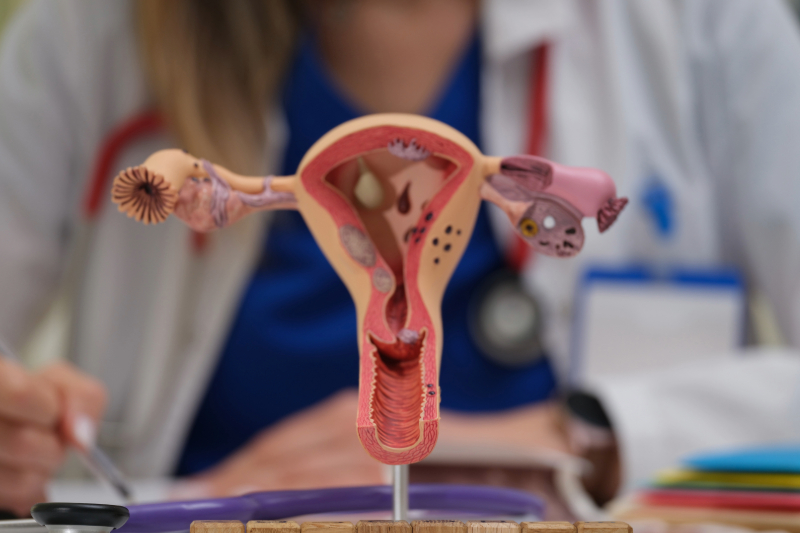
Gynecological Conditions
- Ovarian cysts
- Tubal ligation
- Adhesion removal
- Incision of Bartholin's gland abscess / vaginal cyst
- Pelvic organ prolapse
- Chromoperturbation
- Bartholin's gland cystectomy / vaginal cystectomy
- Curettage biopsy
Oncological Diseases
- Cancer staging
- Omentectomy
- Pelvic and periaortic lymphadenectomy
- Ovarian transposition before irradiation
Have you noticed discomfort, pelvic pressure, or an unusual sensation? Genital prolapse, a common but often overlooked condition, can affect your quality of life. At VenArt Clinic, we offer clear information, personalized solutions, and support to help you regain your comfort and confidence.
Learn everything you need to know about causes, symptoms, and modern treatments to take the first step toward a healthier life!
Book an Appointment
Genital prolapse
Genital prolapse occurs when the supporting structures of the pelvic floor lose their ability to keep the pelvic organs in their normal anatomical position. This dysfunction can lead to the displacement or descent of organs such as the uterus, vagina, bladder, or intestine.
Although it is not a life-threatening condition, genital prolapse often causes discomfort, a feeling of pelvic pressure, or pain, affecting patients’ quality of life.
Uterine prolapse
Uterine prolapse, also known as “dropped uterus,” involves the uterus slipping from its normal position toward the vaginal opening or even outside of it. It is classified according to severity:
- Stage I – the uterus is descended but remains in the upper portion of the vagina;
- Stage II – the uterus reaches the level of the vaginal introitus;
- Stage III – the uterus protrudes outside the vagina, a condition also known as procidentia.
Vaginal prolapse
Vaginal prolapse is an advanced form of vaginal wall descent, which can also occur after a hysterectomy (removal of the uterus). In these cases, the tip of the vaginal stump can descend to or beyond the introitus, resulting in grade II or III vaginal prolapse.
Causes of genital prolapse
Pelvic organ prolapse is the result of a weakening of the structures that hold these organs in place, and this imbalance can be triggered by a number of factors. Among the most common causes are:
- Natural childbirth;
- Aging;
- Excessive body weight;
- Genetic inheritance;
- Intense or prolonged physical exertion;
- Pelvic surgery;
- Chronic diseases;
- Hormonal imbalances.
Clinical manifestations of genital prolapse
Symptoms may vary depending on the severity of the prolapse and the organs involved. Many patients describe a combination of physical discomfort and functional disorders:
- Pressure in the pelvic area: One of the most common symptoms is a feeling of “heaviness” or pressure in the pelvis, which worsens towards the end of the day or after exertion.
- Pelvic pain or discomfort: Pain may occur in the lower abdomen or lower back, especially during exertion or sexual intercourse.
- Perception of a mass in the vagina: Many women notice a bulge or swelling that “protrudes” from the vagina, especially when standing or exerting themselves.
- Urinary problems: These may include difficulty urinating, incomplete bladder emptying, frequent urination, or urinary incontinence during exertion (sneezing, coughing, laughing).
- Bowel problems: Constipation, feeling of incomplete evacuation, or the need to apply pressure to the perineum to defecate are possible symptoms.
- Discomfort during sexual intercourse: Sexual intercourse may become painful due to anatomical changes and abnormal positioning of the pelvic organs.
- Changes in vaginal secretions: Some women notice abnormal vaginal discharge or minor bleeding, especially if the prolapse causes irritation of the vaginal mucosa.
Establishing the diagnosis of pelvic organ prolapse
Correct identification of genital prolapse requires a complex clinical approach that combines symptom assessment with physical examination and, in some cases, additional investigations. The process aims to determine the severity of the condition and rule out other pathologies with similar manifestations.
- Specialist clinical consultation
The first step is an examination by a doctor, who assesses the structure and position of the pelvic organs. This includes external inspection as well as internal vaginal or rectal palpation to observe any descent of the uterus, bladder, or intestines. - Symptomatic history and functional impact
The patient is encouraged to describe her symptoms in detail—from pelvic pressure, urinary difficulties, or constipation to changes in sexual activity. This information is essential to determine whether and to what extent the condition interferes with daily activities. - Additional functional investigations
For a complete understanding of the situation, the doctor may recommend urodynamic investigations (to assess the bladder) or intestinal transit tests, especially if mixed urinary and digestive symptoms are present. - Interdisciplinary consultation
Depending on the case, it may be necessary to involve a gynecologist, urologist, or surgeon specializing in pelvic pathology for a differential diagnosis and the development of a personalized treatment plan. - Advanced imaging techniques
In situations where the clinical examination does not provide sufficient information, methods such as transvaginal ultrasound or pelvic MRI may be used. These provide a detailed image of the organs and their position in relation to adjacent structures.
Treatment options for pelvic organ prolapse
In mild forms of prolapse, especially when there are no symptoms or they are minimal (grade I or II), active medical intervention is not always necessary. In these cases, regular monitoring and lifestyle changes may be sufficient to keep the condition under control.
For advanced forms (grade III) or when discomfort is significant, there are two main treatment options: conservative and surgical.
Conservative treatment
In cases where the perineal structures can adequately support a device, your doctor may recommend the use of a vaginal pessary—a silicone or latex ring inserted into the vagina to support the pelvic organs and reduce the feeling of pressure or prolapse. This method is especially useful for patients who cannot or do not want to undergo surgery.
Surgical intervention
When symptoms persist, affect daily activities, or do not respond to conservative treatment, surgery is considered. As a rule, this involves:
- Removal of the uterus (hysterectomy) in cases of advanced uterine prolapse;
- Reconstruction of the vaginal wall (colporrhaphy) to strengthen weakened areas;
- Fixing the vaginal stump to a solid structure (sacrospinous ligaments or pelvic fascia) to prevent recurrence.
Before surgery, any lesions of the vaginal mucosa (such as ulcers) must be completely healed.
Treatment of post-hysterectomy vaginal prolapse
Cases of vaginal prolapse are managed using techniques similar to those used for uterine prolapse, taking into account the absence of the uterus and adapting the method of suspending the vaginal stump.
Why Choose VenArt Clinic?
Trusted expertise, advanced technology, and care that puts you first — learn more about what sets our gynecology medical services apart:
- Experienced medical team: Specialists with years of practice in gynecology, with proven results and numerous positive testimonials.
- Modern technology: We use minimally invasive methods, such as laparoscopic surgery, for quick recovery and reduced discomfort.
- Personalized approach: Each patient is unique, and the treatment plan is tailored to their needs for a safe and effective medical experience.
- Comprehensive post-operative care: We provide guidance throughout recovery, careful monitoring, and answer any questions to ensure a complication-free healing process.
Medical Team
Frequently Asked Questions
Is prolapse a dangerous condition?
Although not life-threatening, prolapse can significantly affect quality of life through pain, discomfort, and urinary or digestive disorders. Left untreated, it can worsen over time.
Can this condition be prevented?
Yes. By strengthening the pelvic muscles (Kegel exercises), maintaining a healthy weight, avoiding constipation, and avoiding heavy lifting, the risk can be significantly reduced.
Is surgery always necessary?
No. In mild cases, prolapse can be managed through strengthening exercises, the use of vaginal weights, or local hormone therapy. Surgery is recommended in severe cases or when conservative methods are unsuccessful.







