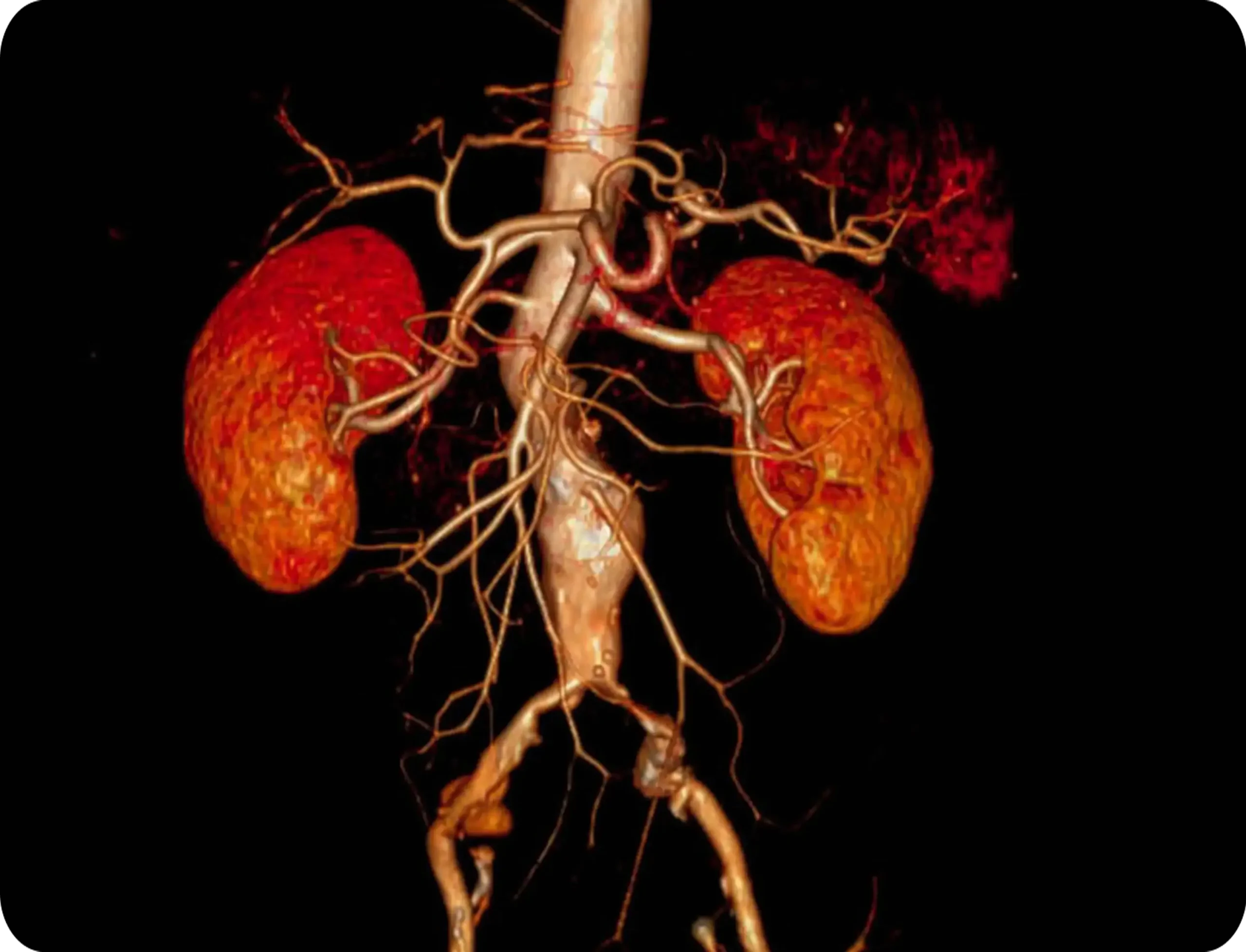
In some complex vascular cases, patients may suffer from extensive arterial disease, such as aneurysms, involving both the aorta and the iliac arteries. In such situations, the primary goal is to re-establish healthy blood flow to the affected areas. Achieving this may require a hybrid approach that combines traditional surgery with minimally invasive techniques, depending on each patient’s specific condition.
For abdominal aortic disease, two main approaches are available: open surgery and endovascular treatment (EVAR). The appropriate method is selected based on medical evaluation.
In the case discussed, the common iliac artery lesion required a cross femoro-femoral bypass, performed in the same surgical session as the EVAR.
EVAR (Endovascular Aneurysm Repair)
EVAR is a modern, minimally invasive procedure used to treat abdominal aortic aneurysms. The aorta is the body’s main artery, responsible for carrying blood from the heart to the rest of the body. An aneurysm is an abnormal enlargement of the artery that poses a serious risk of rupture.
Why Is the EVAR Procedure Necessary?
EVAR helps prevent life-threatening ruptures of abdominal aortic aneurysms. During the procedure, a special tube called an endograft is inserted into the artery. This mesh-covered device creates a new path for blood flow, relieving pressure on the weakened artery wall.
The EVAR Procedure
- Patient preparation: The procedure is performed under general anesthesia;
- Incision: The surgeon makes a small incision in the groin to access the femoral artery;
- Catheter insertion: A flexible tube (catheter) is inserted through this incision and guided up to the aneurysm;
- Endograft placement: The endograft is inserted through the catheter and positioned inside the aorta, covering the aneurysmal area. It expands and firmly attaches to the artery wall, redirecting blood flow.
- Closing the incision: After placement of the endograft, the catheter is withdrawn and the incision is closed.
EVAR is an excellent treatment option for high-risk patients, offering reduced recovery time and fewer complications compared to traditional open surgery.

Femoro-Femoral Bypass: A Life-Saving Procedure for Peripheral Arterial Disease
Femoro-femoral bypass surgery is recommended for patients with severe occlusions (blockages) in the iliac arteries. When angioplasty or stenting is not viable or has not succeeded, this surgical solution can help restore blood flow and relieve symptoms.
Indications for Femoro-Femoral Bypass
Your doctor may recommend this procedure if you experience:
- Significant leg pain while walking (claudication)
- Persistent rest pain in the lower limbs
- Signs of potential tissue damage or risk of limb loss
Surgical Technique
This procedure creates a bypass around the blocked iliac artery by connecting the femoral arteries in both legs:
- Incisions are made in the groin area to access each femoral artery.
- A graft (synthetic or venous) is tunneled under the skin to link the arteries.
- The graft is securely attached at both ends to ensure proper circulation.
- The incisions are closed, and the patient is closely monitored.
Postoperative Care
Following the procedure, patients are typically monitored in the hospital for several days. During this time, the medical team ensures the graft functions correctly while managing any pain or discomfort. Ongoing check-ups are essential to ensure the bypass remains open and effective.
Potential Complications
While the femoro-femoral bypass is a safe and well-established procedure, possible complications include:
- Wound infection
- Graft occlusion/blockage
- Reduced blood flow to the legs (limb ischemia)
These risks are minimized through expert surgical technique and attentive postoperative care at VenArt Clinic.
Your Journey to Improved Vascular Health Starts Here
Femoro-femoral bypass offers a reliable and effective solution for patients with severe peripheral artery disease. By rerouting blood around blocked arteries, this surgery can restore circulation, reduce symptoms, and greatly improve quality of life.
At VenArt Clinic, our team successfully performed hybrid surgery to revascularize the affected regions. In many cases, patients may require additional procedures, such as angioplasty or endarterectomy, to address other areas of arterial disease before this step. These complementary treatments, such as angioplasty and/or endarterectomy, are typically less complex and help optimize long-term outcomes.
Medical consultant: Prof. Dr. Jérôme Cau











