Authors: Jérôme Cau, MD; Jean Baptiste Ricco, MD; Olivier Page, MD; Gilles Régnault de la Mothe, MD; Christophe Marchand, MD; Alexandre Valagier, MD; La Poitiers, France
This article is intended for medical professionals. The full article can be found in one of the most prestigious vascular surgery publications: go to article.
Objective
The purpose of this article is to report the achievements of vascular surgery related to this laparoscopic technique and to demonstrate that it is a safe and effective option for treating hypertension and recurrent renal failure. This procedure has been successfully performed in patients whose hypertension was refractory to medical treatment and who failed PTRA due to renal artery restenosis.
Methods
Our surgeons have extensive experience in total laparoscopic repair of renal artery restenosis following PTRA. From February 2005 to October 2009, we performed six total laparoscopic aortorenal bypasses in patients with recurrent hypertension and renal failure.
Results
The mean duration of surgery was 246 minutes, while the warm ischemic time was 28 minutes. All patients underwent prosthetic graft interposition with an estimated surgical blood loss of 980 ml. No conversions to open surgery or deaths occurred during hospitalization.
Postoperative serum creatinine levels initially increased but returned to baseline before discharge. The mean postoperative hospital stay was six days. Patency was confirmed by color Doppler ultrasound and computed tomography (CT) examination. After surgery, hypertension improved, although renal failure remained unchanged.
Conclusion
Total laparoscopic repair is feasible and safe in this setting but requires extensive technical experience in total laparoscopy for successful outcomes. Our team has over two decades of experience in minimally invasive surgery, particularly in advanced laparoscopic procedures such as aortic reconstruction for thoracic or abdominal aneurysms, as well as vascular access for hemodialysis. All these experiences are essential for success in performing total laparoscopic repairs for renal artery restenosis after PTRA.
We use state-of-the-art technology that allows us to operate with greater precision and dexterity than ever before, improving clinical outcomes by minimizing infection risk, reducing operating time, and enhancing patient comfort throughout the process. Our team focuses on optimizing preoperative care and continuously updating our techniques in line with recent evidence-based guidelines to ensure all patients receive the best possible treatment, from diagnosis to recovery.
Materials and Methods
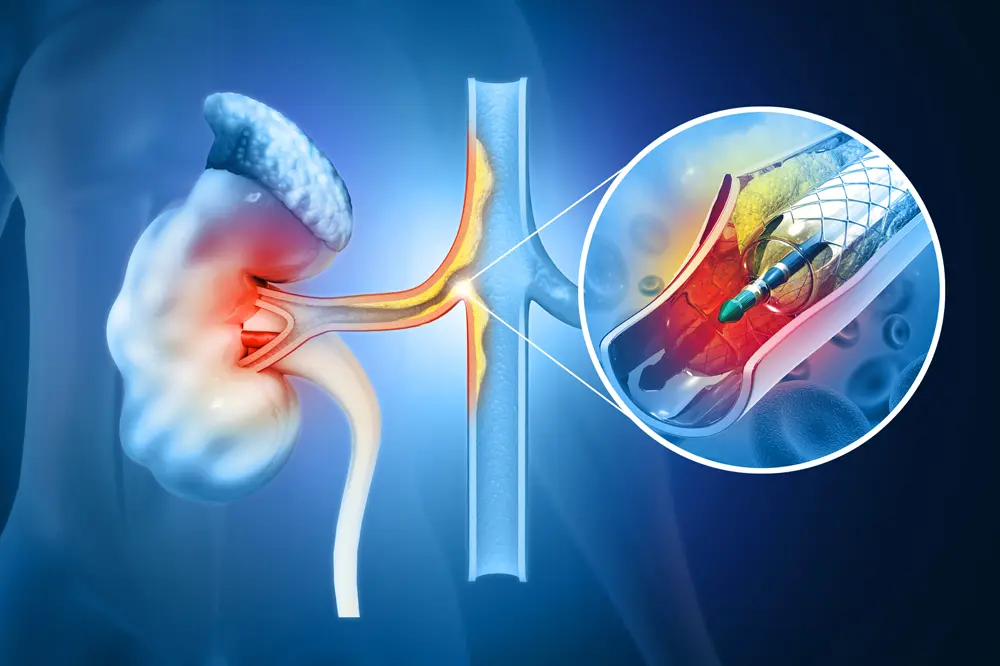
Total laparoscopic bypass (TLB) is a surgical option used to treat renal artery restenosis (RAR). Unlike traditional open surgery, which involves making a large incision in the chest or abdomen and inserting a tube-like graft into the renal artery, TLB requires only two small abdominal incisions. Instruments are inserted directly into the renal artery through these incisions. This approach helps preserve healthy surrounding tissue and reduces postoperative pain compared to open surgery. Furthermore, TLB procedures generally take less time than open surgery, making the experience less stressful for patients and their families, and resulting in shorter hospital stays.
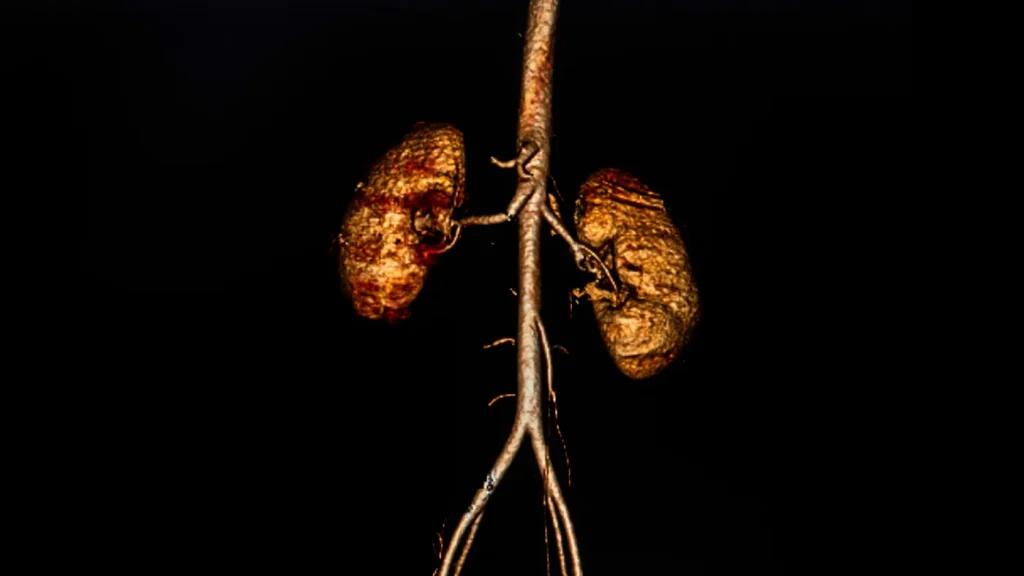
Between February 2005 and October 2007, six patients (four men and two women) underwent total laparoscopic bypass for RAR after PTRA in our department. All six had a preoperative diagnosis of hypertension; four of these cases were associated with at least one episode of acute pulmonary edema.
Three patients had a single functioning kidney; two had severe eGFR <30 ml/min/1.73 m²; and four had moderate eGFR between 30 and 60 ml/min/1.73 m². During the same period, our department performed 92 total laparoscopic aortic bypasses and 66 PTRA procedures.
The success rate of TLB surgery varies depending on factors such as patient age, severity of RAR symptoms before treatment, and degree of vessel involvement before surgery. However, studies have shown that total laparoscopic bypass can improve outcomes compared to conventional open surgery techniques for treating RAR. Therefore, it should be considered an important therapeutic option for patients seeking a minimally invasive solution to this condition.
Results
The bypass surgery demonstrated remarkable postoperative results with no in-hospital deaths. Serum creatinine levels increased during the procedure but returned to baseline at discharge. Data analysis showed a reduction of one antihypertensive medication per patient at six months and one year after bypass surgery compared to preoperative values. Doppler ultrasounds and CT angiography confirmed the success, showing no hemodynamic or morphological problems one year postoperatively.
Discussion
Laparoscopic renal artery bypass is a complex procedure that requires careful dissection of delicate vascular structures. Effective exposure of the right kidney requires a retrocolic approach, while to avoid postoperative complications on the left side, lateral placement of the aorta should be considered when performing anastomoses with other vessels. Precise mobilization and transposition are essential for successful outcomes in this complex operation.
Despite these difficulties, the laparoscopic technique offers advantages such as an improved visual field and better control of the distal renal artery, allowing for more precise dissection and superior conditions for arterial anastomosis. These benefits are comparable to those achieved under magnifying binocular loupes.
Our extensive experience in laparoscopic aortic surgery facilitates the transition to total laparoscopic renal artery bypass. A notable challenge in this procedure is achieving short warm ischemia times, especially in patients with a single functioning kidney who may require multiple bypasses. In this study, successful clamping was achieved within 28 minutes without robotic assistance, demonstrating the skill of our surgical approach.
Renal artery clamping time remains a critical factor, as renal ischemia must be minimized, particularly in cases with single functioning kidneys. The average clamping time of 28 minutes was accomplished through our extensive experience in laparoscopic aortic surgery without robotic devices.
Since we routinely perform laparoscopic aortobifemoral bypass, the laparoscopic approach to the renal arteries did not present additional challenges. Nonetheless, total laparoscopic renal bypass remains technically demanding. Prior training and experience in total laparoscopic aortic surgery, involving more than 50 successful cases, is likely necessary to achieve good outcomes.
Unfortunately, laparoscopic aortic surgery is not widely adopted, making experience difficult to gain. In 2008, only 1,073 patients underwent laparoscopic aortic surgery worldwide. This limited adoption is due primarily to the time-consuming training required and the difficulty in identifying suitable patients for whom laparoscopic surgery would be preferable to endovascular techniques.
Given these factors, recommending laparoscopic renal artery surgery is difficult, even though it yields good results for a small number of well-trained and motivated surgeons.
Despite technical challenges, good outcomes can be achieved with sufficient training and experience. However, adoption of this technique has been slow due to the steep learning curve and limited case availability.
Final Conclusion
Total laparoscopic renal artery bypass is feasible but remains technically challenging. Prior experience in total laparoscopic aortic surgery is essential before undertaking this procedure.
Medical Consultant: Jérôme Cau