What Are Venous Stents?
Venous stents are metal mesh tubes used to open narrowed or blocked veins. They act as a scaffold, supporting the vein walls to keep them open and restore blood flow. Typically, venous stents are placed in larger central veins, such as those located in the legs, chest, or abdomen. These stents help treat vein narrowing caused by various conditions that restrict normal blood circulation.
What Conditions Are Treated With Venous Stents?
Doctors recommend venous stents for chronic blood clots or other conditions that compress or narrow veins, limiting blood flow. At VenArt Clinic, venous stents are used to treat several conditions, including chronic deep vein thrombosis. This condition involves blood clots forming in large, deep veins that reduce the amount of blood returning to the heart and lungs from the leg or sometimes the arm.
Post-Thrombotic Syndrome
Post-thrombotic syndrome can damage veins after a blood clot has occurred. Symptoms may develop over years and include swelling of the affected limbs and chronic pain. If you have suffered deep vein thrombosis, it may take a long time before you notice signs of post-thrombotic syndrome, which can significantly impact quality of life.
May-Thurner Syndrome
May-Thurner syndrome occurs when the right iliac artery presses on the left iliac vein. This pressure causes narrowing and scarring of the vein, which leads to chronic swelling, pain, and fatigue in the left leg. The compression results from the artery crossing over and compressing the vein inside the pelvis.
Nutcracker Syndrome
Nutcracker syndrome arises when arteries near the kidney compress the left renal vein. This compression causes blood to flow backward, resulting in pain in the left side of the abdominal wall (flank pain) and sometimes blood in the urine. The syndrome affects vein drainage from the kidney and can cause significant discomfort.
Hemodialysis/Arteriovenous Fistulas
If you are undergoing hemodialysis and experience reduced blood flow in your grafts or fistulas, venous stents may be recommended. Stents help open central veins in the chest, improving drainage and maintaining access for dialysis treatment. Proper vascular access is vital to the success and safety of hemodialysis therapy.
How To Prepare For The Venous Stent Placement Procedure
Your vascular surgeon will take a detailed medical history and perform a physical examination. Depending on your situation, imaging tests such as ultrasound may be ordered to visualize your blood vessels. Your doctor may also request a venogram, an X-ray procedure that maps the anatomy of your veins. These tests help identify any narrowing or blockages precisely, guiding the planning of the stent placement.
How Is The Venous Stent Placement Procedure Performed?
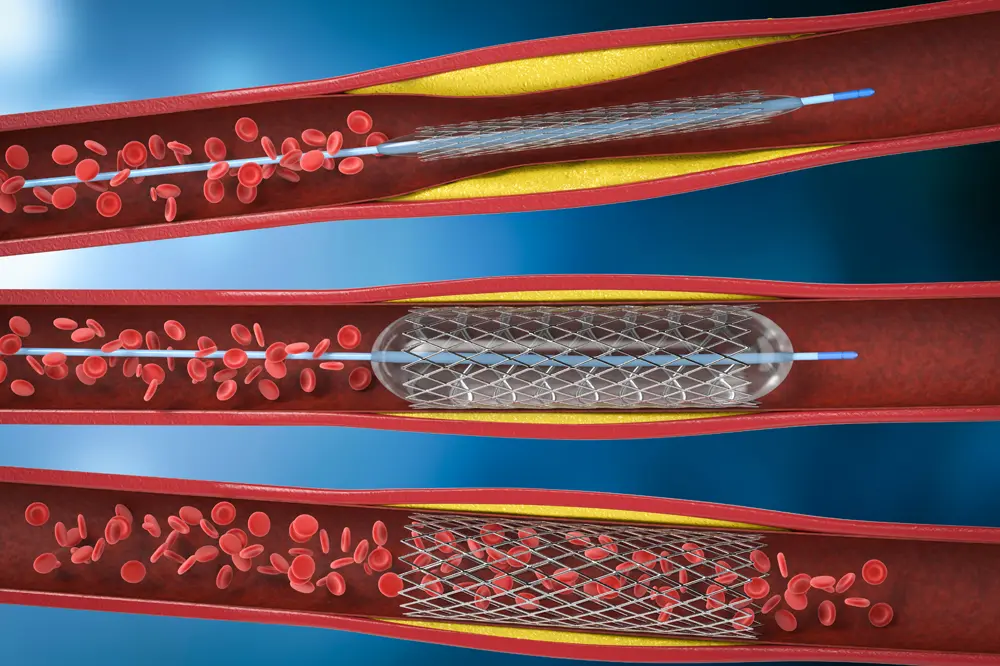
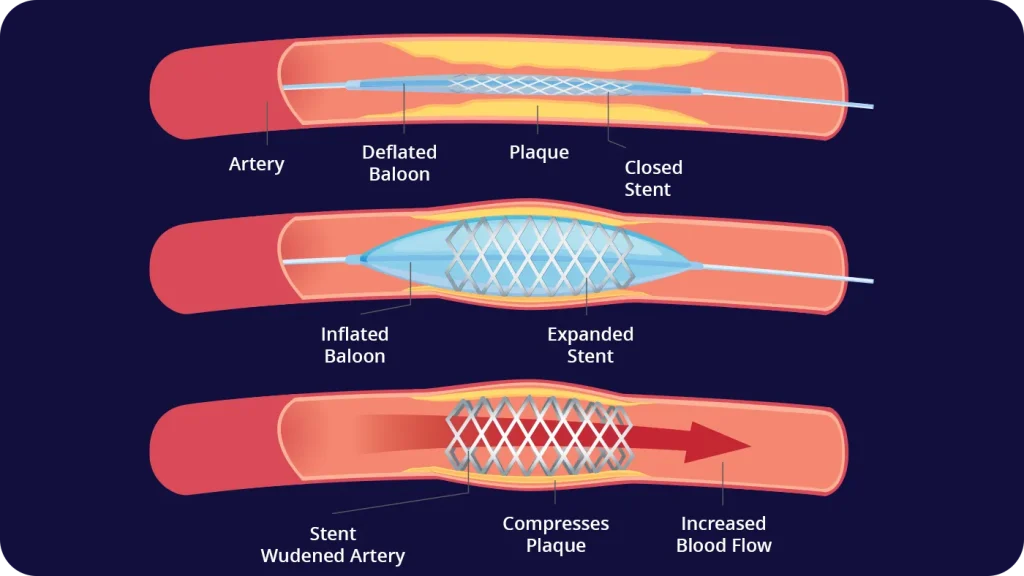
Moderate sedation is generally sufficient to place venous stents. However, if your veins contain clots or other obstructions, your doctor may first perform angioplasty. This minimally invasive procedure widens narrowed or blocked veins by inflating a balloon inside the vessel.
The doctor begins by inserting a needle into a vein, typically in the groin or behind the knee depending on the affected area. A guide wire is advanced through the needle, followed by a catheter sheath and a guide catheter. Fluoroscopy, or real-time X-ray imaging, helps the doctor guide these instruments to the narrowed or blocked vein.
Once positioned, a balloon catheter is inflated and deflated multiple times to dilate the vein. After adequate widening, the balloon is removed, and a catheter carrying a closed stent is advanced and deployed in the vein. The stent pushes the vein walls outward, acting as a scaffold to keep the vessel open. Finally, the catheters are withdrawn, and pressure is applied to the puncture site to stop bleeding and close the wound.
How Long Is The Hospital Stay And Recovery After The Stenting Procedure?
Recovery following angioplasty and stenting is typically brief. Most patients are discharged from the hospital within 12 to 24 hours after catheter removal. Many return to normal activities or work within a few days to a week. Your doctor will provide specific post-procedure care instructions to ensure safe and efficient healing.
Why Choose VenArt Clinic For A Venous Stent?
VenArt Clinic is a leader in treating vascular conditions. We offer a full range of minimally invasive arterial and venous treatments alongside traditional surgical procedures such as carotid surgery. Our team of doctors has decades of experience and advanced training in Europe and the United States.
If venous stenting is not the optimal treatment for your condition, we will recommend alternatives tailored to your individual needs and health status. If you wish to schedule a consultation or learn more about venous stenting, please contact us.
Medical Consultant: Prof. Dr. Jérôme Cau