A hiatal hernia is the protrusion or turning of the upper part of the stomach into the chest cavity through the diaphragmatic (hiatal) opening that connects it to the abdominal cavity.
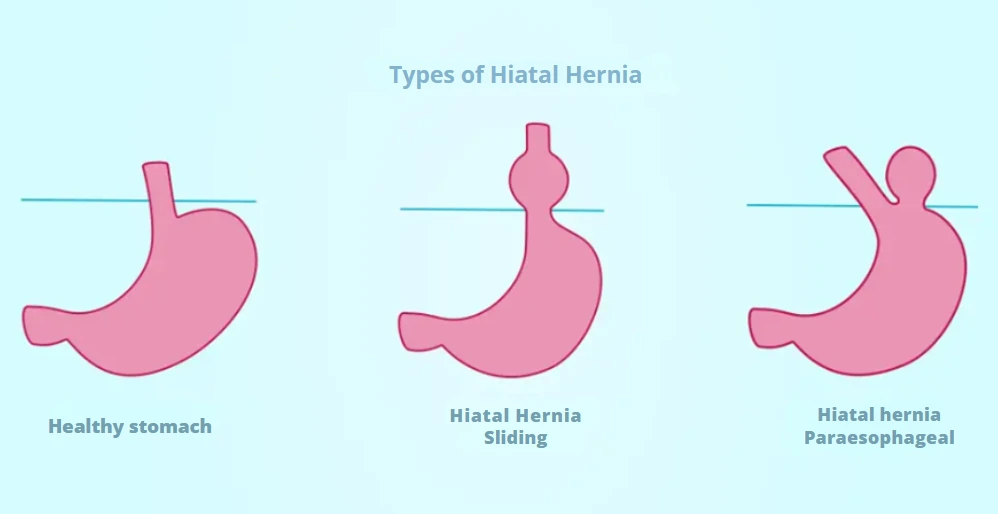
What Are the Types of Hiatal Hernias?
- Sliding – turning of the esophagogastric junction;
- Paraesophageal – turning of a portion of the stomach;
- Mixed – a combination of the two above.
The most common type is sliding. Paraesophageal hernias are less frequent but can cause serious complications such as strangulation or obstruction. Hernias can also be classified by size. Small hiatal hernias often do not cause symptoms, while large hernias may allow stomach contents to return to the upper digestive tract, causing discomfort.
What Are the Symptoms and Complications of Hiatal Hernia?
Most small hernias are asymptomatic. Large hiatal hernias can cause:
- Burning sensation in the stomach (heartburn), worsened by bending forward or lying down;
- Chest or abdominal pain, often after meals;
- Regurgitation of food or liquids;
- Return of stomach acid into the esophagus;
- Difficulty swallowing;
- Difficulty breathing;
- Vomiting blood, resembling coffee grounds, or black stools indicating gastrointestinal bleeding;
- Feeling of fullness and early satiety during meals.
Complications include bleeding, which may cause fatigue due to blood loss. Bleeding occurs when the digestive tract is damaged by the edges of the diaphragmatic opening. Paraesophageal hernias can become incarcerated, reducing blood flow to the stomach wall and causing strangulation. Immediate medical attention is required in these cases.
What Are the Causes of Hiatal Hernia?
The exact cause is not fully known. Factors that may contribute include:
- Injuries, trauma, or previous surgery;
- High abdominal pressure caused by lifting heavy objects, childbirth, or obesity (Recommended article: What are the benefits of bariatric surgery);
- Presence of an enlarged diaphragmatic ring at birth.
Additional risk factors include smoking and advanced age.
How Is Hiatal Hernia Diagnosed?
Diagnosis begins with a review of symptoms. Paraclinical diagnostic methods may include:
- Upper digestive endoscopy – a thin tube with a camera is inserted into the mouth to examine the esophagus and stomach;
- Barium X-ray – drinking a barium solution allows X-ray imaging to visualize the digestive tract.
What Are the Treatment Options for Hiatal Hernia?
Treatment depends on symptom severity and may involve medication or surgery.
Medication
Medications aim to relieve heartburn and acid reflux:
- Antacids to neutralize stomach acid;
- Drugs that reduce acid production;
- Drugs that block acid production and allow the esophagus to heal.
Surgery
Surgery is recommended if symptoms are severe, medication fails, or complications are likely. VenArt Clinic specializes in general surgery, including hiatal hernia repair.
How Is the Surgery Performed?
Hiatal hernia repair can be performed using open surgery, laparoscopic surgery, or endoluminal surgery. General anesthesia is required for all approaches.
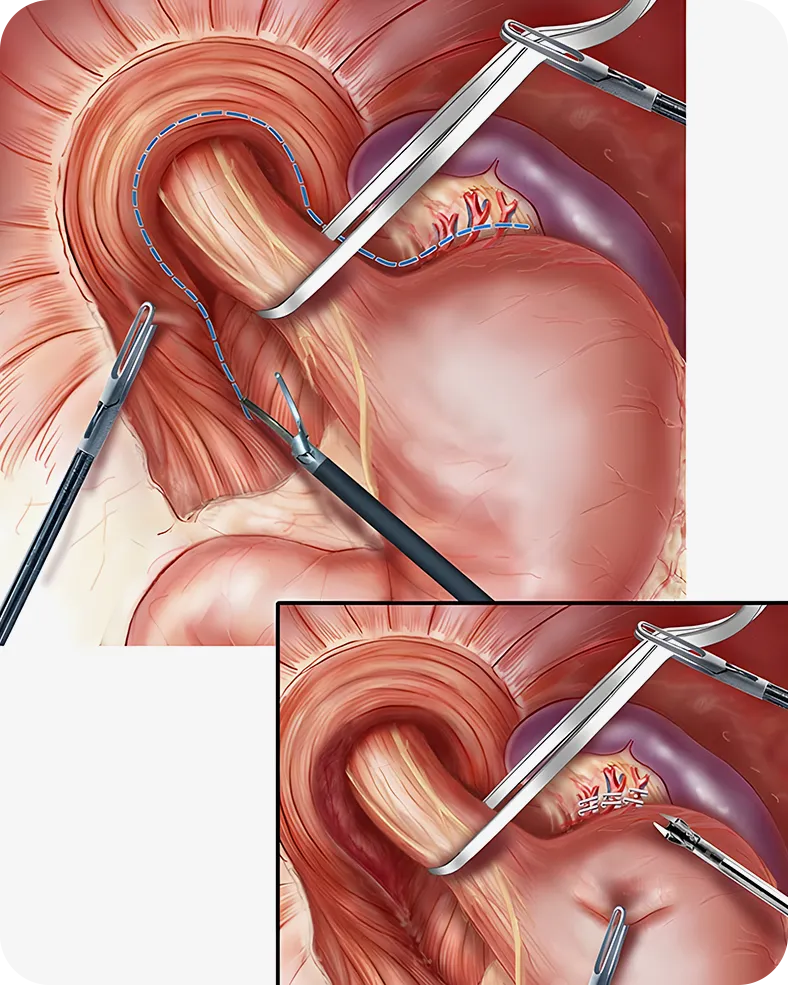
Laparoscopic Surgery
This minimally invasive procedure uses small abdominal incisions. A laparoscope with a camera is inserted, the hernia is repaired, and the diaphragmatic opening may be reinforced. Advantages include:
- Lower risk of infection;
- Less pain;
- Smaller scars;
- Faster recovery;
- Better results.
Open Surgery
This involves a larger incision to reposition the stomach and wrap it around the distal esophagus, strengthening the digestive tract walls and preventing acid reflux.
Endoluminal Fundoplication
Endoluminal fundoplication is a newer, minimally invasive procedure. No incisions are required; an endoscope is inserted through the esophagus. The surgeon attaches small clips at the junction of the esophagus and stomach to prevent acid and food from returning to the esophagus. This procedure is suitable only for selected patients.
Preventing hiatal hernia is challenging. Patients are advised to reduce risk factors: avoid a sedentary lifestyle, do not lie down immediately after meals, and wait 2–3 hours before engaging in physical activity.
Dr. Oleg Cebotari, PhD candidate in Medical Sciences, has completed extensive postgraduate training in Romania and Heidelberg, Germany. He performs classical and laparoscopic surgeries with exceptional results and is a recognized leader in his field.
Symptoms of Hiatal Hernia
Sliding hiatal hernias are usually asymptomatic but may cause chest pain or GERD symptoms. Paraesophageal hernias can be silent but may become incarcerated or strangulated. Both types can cause massive or occult gastrointestinal bleeding.
Diagnosis of Hiatal Hernia
Large hiatal hernias are often detected on chest X-ray. Small hernias are diagnosed by barium swallow.
Hiatal Hernia Can Be Classified as Follows
- Sliding (axial, cardio-esophageal) – the cardia passes into the thorax with the stomach;
- Rolling (paraesophageal) – the stomach bottom passes into the thorax without the cardia;
- Mixed – combination of both types.
Complications of Paraesophageal Hernia
Common complications include digestive microhemorrhages, causing secondary anemia, observed in 55% of cases. Ulcers may develop on the herniated stomach portion, potentially leading to bleeding or perforation. Gastric volvulus, or twisting of the stomach, presents with:
- Intense pain;
- Ineffective vomiting;
- Inability to place a gastric tube.
If strangulation occurs, patients may experience chest symptoms and difficulty breathing. Necrosis with perforation has a 50% mortality rate.
Medical Consultant: Dr. Oleg Cebotari











