Total laparoscopic repair of restenosis renal artery after percutaneous transluminal renal stenting (PTRA)
- Medically checked
Home » Total Laparoscopic Repair for Restenosed Renal Artery After Percutaneous Transluminal Renal Angioplasty (PTRA) with Stenting
Medical Procedures
Laparoscopic Interventions
Classic Surgical Interventions
Conditions Treated
Abdominal Conditions
- Gallbladder Disease
- Tumors of the Stomach, Liver, Pancreas
- Intestinal Pathologies
Pelvic and Perineal Conditions
Other Conditions Treated
- Thyroid
- Abdominal Lymphadenectomies
- Esophageal Tumors
Objective
The purpose of this article is to report the achievements of vascular surgery related to this laparoscopic technique and to prove that it is a safe and effective option for treating hypertension and recurrent renal failure. This procedure has been successfully performed in patients whose hypertension was refractory to medical treatment and who failed PTRA due to renal artery restenosis.
Methods
Our surgeons have had extensive experience in the total laparoscopic repair of renal artery restenosis following PTRA. From February 2005 to October 2009, we performed 6 laparoscopic total laparoscopic aortorenal aortorenal bypasses in these patients with recurrent hypertension and renal insufficiency.
Results
The mean operative time was 246 minutes, while the warm ischemic time was 28 minutes. All patients underwent prosthetic graft interposition with an estimated surgical blood loss of 980 mL; no conversions or deaths occurred during hospitalization.
Our patients’ postoperative serum creatinine levels increased but returned to baseline before discharge; mean postoperative length of hospital stay at 6 days; patency was confirmed by color Doppler ultrasonographic and computed tomography (CT) scans. After surgery, hypertension improved, although renal insufficiency remained unchanged.
Conclusion
Total laparoscopic repair is thus feasible and safe in this setting, but requires extensive technical expertise in total laparoscopy for successful results. Our team has more than two decades of experience in minimally invasive surgery, especially in advanced laparoscopic procedures such as aortic reconstruction on thoracic or abdominal aneurysms, as well as vascular access for hemodialysis; all these experiences are essential elements for success in performing total laparoscopic repair for renal artery restenosis laparoscopic total laparoscopic repair after PTRA.
We use state-of-the-art technology that allows us to operate with greater precision and dexterity than ever before, improving clinical outcomes by minimizing the risk of infection, reducing operative time and improving patient comfort throughout the process. Our team is also focused on optimizing preoperative care and continually updating our techniques in line with recent evidence-based guidelines, so that all of our patients receive the best possible treatment from diagnosis through recovery.

Materials and methods
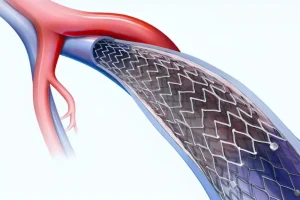
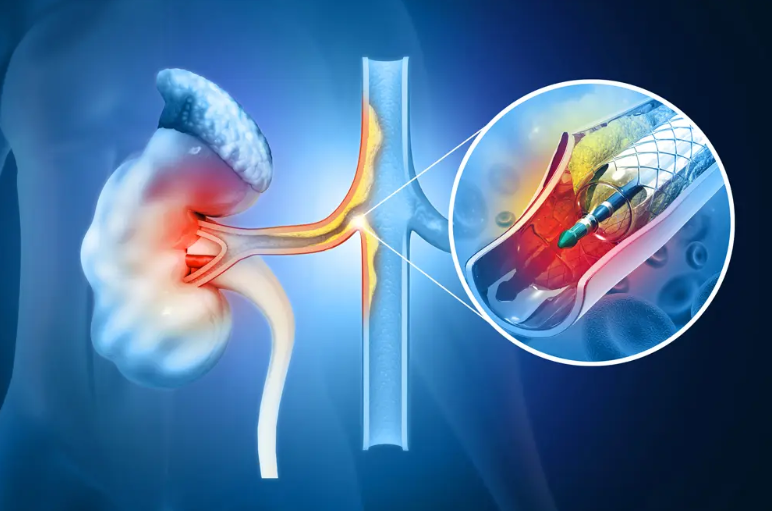
Total laparoscopic bypass (TLB) is one such surgical option used to treat renal artery restenosis (RAR). Unlike more traditional open surgery, which involves making an incision in the chest or abdomen and then inserting a tube-like graft into the renal artery, TLB requires only two small incisions in the abdomen, through which instruments are inserted directly into the renal artery. This helps preserve surrounding healthy tissue and reduces postoperative pain compared to open surgery. In addition, TLB procedures typically take less time than open surgery – making them less stressful for patients and their families – and result in shorter hospital stays.
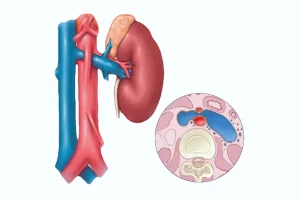
Between February 2005 and October 2007, 6 patients (4 men and 2 women) underwent total laparoscopic bypass for RAR after PTRA in our department. All 6 had a preoperative diagnosis of hypertension associated with at least one episode of acute pulmonary edema in 4 cases; 3 had one functioning kidney; 2 had severe eGFR <30 ml/min/1.73 m2); 4 moderate eGFR (30 to 60 ml/min/m2). During the same time period, 92 laparoscopic total laparoscopic aortic bypasses and 66 PTRAs were performed in our department.
The success rate of TLB surgery varies depending on several factors, including the patient’s age, the severity of RAR symptoms before treatment, the degree of vessel damage before surgery, etc. In general, however, studies have shown that total laparoscopic bypass can improve outcomes compared to conventional open surgical techniques for treating RAR. As such, it should be considered an important therapeutic option for those seeking a minimally invasive solution when faced with this condition.
Results
The bypass surgery showed remarkable postoperative outcomes with no in-hospital deaths. Serum creatinine levels increased during the procedure but returned to baseline at discharge. A notable improvement was a decrease of 1 antihypertensive drug per patient from preoperative values at 6 months and 1 year after bypass surgery, according to data analysis. Doppler ultrasound as well as CT angiography confirmed this success with no hemodynamic or morphologic problems elevated 1 year later.
Discussion
Laparoscopic renal artery bypass is a difficult procedure requiring careful dissection of delicate vascular structures. Efficient exposure of the right kidney requires the use of a retrocolic approach, while to avoid any postoperative problems in left cases, placement on the lateral side of the aorta should be considered when anastomosing other vessels. Mobilization and precise transposition are essential steps for successful outcomes involving this complex operation. However, despite these difficulties, the laparoscopic technique offers some advantages, such as an improved field of view and better control of the distal renal artery, allowing more precise dissection and better conditions for arterial anastomosis, comparable to that completed under binocular magnifying loupe.
We have considerable experience in laparoscopic aortic surgery, which makes the transition to laparoscopic total renal artery bypass grafting easier for our team. However, there is an inherent challenge in achieving short warm ischemia times during this complex procedure – especially if multiple bypasses have been performed in a patient with a single functioning kidney. In this study specifically, we achieved successful clamping in 28 minutes. This was accomplished without using the assistance of a robotic device and is a testament to the competence of our surgical approach.
Renal artery clamping time is another challenge of laparoscopic total renal artery bypass because renal ischemia needs to be as short as possible, especially in this situation where 3 bypasses were performed in patients with only one functioning kidney. In this study, the mean clamping time was 28 minutes, this was achieved without any robotic device due to our extensive experience in laparoscopic aortic surgery.
Because we routinely perform laparoscopic aortobifemoral bypass, the laparoscopic approach to the renal arteries did not present a challenge for us. However, we agree that laparoscopic total laparoscopic renal bypass remains technically demanding and that prior training and experience in total laparoscopic laparoscopic aortic surgery with more than 50 successful cases is probably required to achieve these good results. Unfortunately, laparoscopic aortic surgery is not a popular technique and as such gaining experience can be difficult. Laparoscopic aortic surgery has been adopted by only a few surgeons and the number of patients operated on remains small. In 2008, we identified only 1073 patients who underwent laparoscopic aortic surgery. This can be explained firstly by the need for time-consuming training and secondly because it is increasingly difficult to identify patients in whom laparoscopic aortic surgery would be the preferred technique over endovascular techniques.
It is therefore difficult to recommend laparoscopic renal artery surgery, even if it works well for a small number of well-trained and motivated surgeons.
Despite the technical requirements of laparoscopic total laparoscopic renal bypass, good results can be achieved with sufficient training and experience in laparoscopic aortic surgery. However, adoption of this technique has been slow as few surgeons have followed it due to the extended learning curve – in 2008, only 1073 patients underwent laparoscopic aortic surgery. Of course, such figures also reflect the fact that gaining access to training and identifying suitable cases for such surgery is becoming increasingly difficult.
The bottom line
Laparoscopic total renal artery bypass is feasible. However, it remains technically difficult and previous experience in laparoscopic total aortic surgery is essential before embarking on this technique.