Peripheral Arterial Disease and Arterial Ischemia: Causes, Symptoms, Complications, and Treatment
- Medically checked
Home » Peripheral arterial disease. Arterial ischemia. Causes, symptoms, complications, treatment
Medical Procedures
Laparoscopic Interventions
Classic Surgical Interventions
Conditions Treated
Abdominal Conditions
- Gallbladder Disease
- Tumors of the Stomach, Liver, Pancreas
- Intestinal Pathologies
Pelvic and Perineal Conditions
Other Conditions Treated
- Thyroid
- Abdominal Lymphadenectomies
- Esophageal Tumors
Peripheral Arterial Disease (PAD), also known as Peripheral Vascular Disease (PVD), is a common condition affecting about 20% of people over the age of 65 in many developed countries. PAD results from atherosclerosis—when cholesterol builds up inside the arterial walls, hardening and narrowing the arteries.
This buildup forms plaques that restrict blood flow, leading to serious complications. When blood can’t reach the legs properly due to partially or fully blocked arteries, walking becomes painful and, in severe cases, may result in gangrene or leg amputation.
What Are the Symptoms of Peripheral Arterial Disease?
- Cramping in the legs, especially the calves and thighs, during walking or physical activity
- Pain that disappears when you rest
- Numbness or tingling in the legs and feet
- Sharp, shooting pain in the feet, especially while resting
- A constant feeling of muscle fatigue or “muscle fever” in the leg
- Cold feet or one foot colder than the other
- Loss of leg hair
- Changes in skin color on the foot or toes
- Pain that wakes you up at night
Recommended article: The Venosteam steam method has remarkable advantages over other thermal methods of varicose vein treatment
Important Note: Many older adults assume these symptoms are simply signs of aging. However, they are often linked to PAD. It’s essential to speak with your doctor. An arterial Doppler examination is critical to detect the problem early, begin proper treatment, and prevent serious complications.
Who’s Affected?
PAD affects approximately 10% of the population, which varies by country, diet and lifestyle. It can affect anyone but is more common in individuals over age 50.
Risk Factors in Peripheral Arterial Disease
The people most at risk include:
- Adults over 50
- Smokers
- Diabetics
- Individuals with a sedentary lifestyle
- Overweight individuals
- Patients with high blood pressure or high cholesterol
- Anyone with a family history of peripheral arterial disease
How Peripheral Arterial Disease Is Diagnosed
To diagnose PAD, your doctor may recommend the following:
- Echo-Doppler: Measures blood flow and identifies any blockages
- Ankle-Brachial Index: Compares blood pressure in the ankle to the arm; lower ankle pressure suggests narrowed or blocked arteries
- CT Angiography or MRI Angiography: Visualizes the arteries
- Magnetic Resonance Imaging (MRI): Provides detailed views of arterial narrowing, blockages, aneurysms, and calcifications
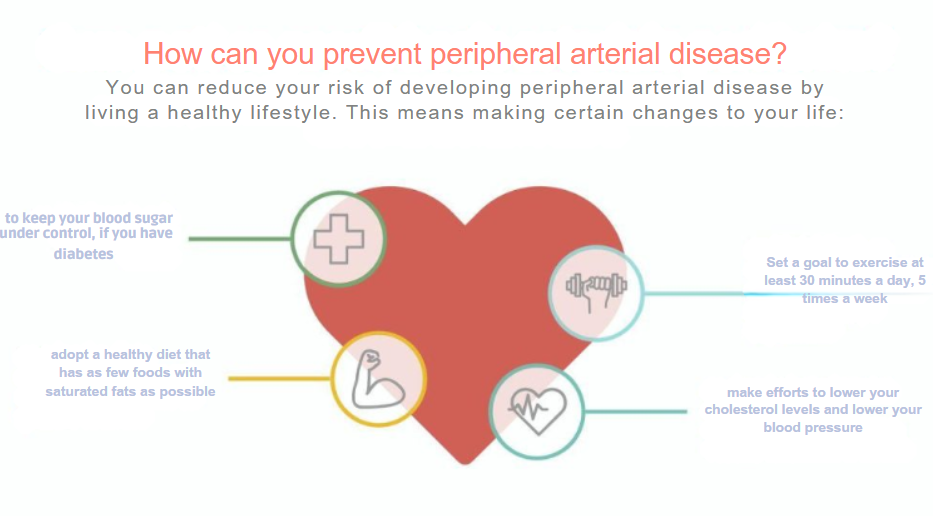
How to Prevent Peripheral Arterial Disease
If you notice any symptoms of peripheral arterial disease, talk to your doctor right away. Early diagnosis can help reduce symptoms and improve the success of treatment. Lifestyle changes, early medication, and vascular monitoring play a key role in prevention.
Peripheral Arterial Disease Complications
If left untreated, PAD can lead to serious and life-threatening complications. Reduced blood flow not only affects the legs but may also indicate broader vascular issues, including heart disease and stroke. Timely diagnosis and treatment are essential.
Peripheral Arterial Disease, Arterial Ischemia – Treatment
Medication
Treatment may include cholesterol-lowering and blood pressure medications, as well as drugs that prevent clotting or reduce arterial plaque buildup.
Peripheral Arterial Disease Endovascular Treatment
Angioplasty and Stenting
Angioplasty and stenting are performed using advanced imaging guidance. The doctor gently inserts a thin catheter through the femoral artery in the groin and guides it to the area where the artery is narrowed or blocked. Once in place, a small balloon is inflated to reopen the artery and restore healthy blood flow. In some cases, a stent—a small mesh cylinder made of metal wires—is inserted to keep the artery open. This procedure is minimally invasive and does not involve traditional surgery. It only requires a small puncture about the size of a pencil tip.
Balloon angioplasty and stenting have largely replaced open surgery as the preferred treatment for Peripheral Arterial Disease (PAD). Large, randomized clinical trials around the world have shown that for many types of arterial blockages, this approach is just as effective as surgery. Recovery is much faster—most patients are able to leave the clinic within 24 hours or less. Because of its proven safety, effectiveness, and quick recovery time, angioplasty and stenting is now considered the first-line treatment for peripheral arterial disease.
Atherectomy
Atherectomy is a minimally invasive treatment used to remove plaque buildup inside the arteries. During this procedure, the doctor inserts a small catheter into the affected artery. At the site of the blockage, the catheter is equipped with a special tool that either shaves or cuts away the plaque. This allows the artery to be cleared and blood flow to be restored without the need for open surgery.
Stent-Graft
A stent-graft is a special type of stent made from metal mesh and covered with a synthetic material. It is shaped like a tube and is used to reinforce a weakened or damaged artery, typically in the case of an aneurysm. Blood pressure and other stressors can cause the wall of the artery to bulge like a balloon, increasing the risk of rupture over time.
The stent-graft acts as a support structure, sealing and stabilizing the weakened artery wall. It spans the length of the aneurysm—from just below it to just above—allowing blood to flow smoothly through the graft without putting pressure on the damaged section of the artery. This treatment is commonly used for abdominal aortic aneurysms (AAA), thoracic aortic aneurysms (TAA), and occasionally for other types of aneurysms.
Aneurysms most often develop in the aorta, the largest artery in the body. Normally, the aorta measures around 2 centimeters in diameter. Aneurysms are diagnosed when the artery’s diameter increases by at least 1.5 times its normal size. A ruptured aortic aneurysm is a life-threatening emergency, as it causes severe internal bleeding and can be fatal if not treated immediately by a specialized medical team.
The formation of aneurysms is often linked to hardening of the arteries—a sign of advanced vascular disease, which also includes conditions like heart attack and stroke. When detected early, these issues can often be managed with lifestyle changes. Quitting smoking and committing to a regular exercise routine can help relieve symptoms and slow disease progression.
Endovascular stent-grafts are designed specifically to prevent aneurysms from rupturing. The term “endovascular” means that the procedure is performed from within the blood vessel. Using specially designed instruments, the vascular surgeon makes a small incision in the artery and inserts a thin tube (catheter) that carries the stent-graft to the aneurysm site. Once in position, the stent-graft is deployed to stabilize, realign, and reinforce the artery from within.
Patients usually recover faster from endovascular treatment than from traditional surgery. Hospital stays are shorter, and the risk of complications is lower due to the minimally invasive nature of the procedure. However, in certain cases—such as when the shape or location of the aneurysm is not suitable for stent placement—traditional open surgery may still be the safer and more effective option.
How to Prepare for Stent-Graft Treatment
Your doctor will begin by reviewing your medical history and performing a thorough physical examination. In addition, you may be asked to undergo several diagnostic tests. These can include an electrocardiogram (ECG), an exercise stress test, and an Angio Scan (MRI or CT). These imaging studies help determine the size, shape, and location of the aneurysm, which are essential in deciding whether endovascular stent-grafting is a suitable treatment option.
If the evaluation confirms that stent-graft treatment is appropriate, your doctor may recommend additional, more detailed investigations:
- Spiral CT scan: This test uses a series of rapid X-rays taken in a spiral pattern around your body. A computer then reconstructs a three-dimensional image of your blood vessels for precise assessment.
- Angiography: In this procedure, a thin catheter is inserted into an artery. A contrast dye is then injected through the catheter, and X-ray images are taken to provide detailed pictures of the blood vessels.
These tests help your doctor plan the safest and most effective treatment tailored to your condition.
Am I Eligible for Endovascular Stent-Graft?
You may be eligible for endovascular stent-grafting if the aortic aneurysm is large enough—typically more than 5 centimeters in diameter—and there are healthy sections of artery both above and below the aneurysm where the stent-graft can be securely placed. This minimally invasive option is especially beneficial for patients at higher risk of complications from conventional surgery due to other existing health conditions.
However, if you have a long life expectancy, a low surgical risk, or if the shape or location of the aneurysm is not favorable for endovascular repair, traditional open surgery may be recommended. At VenArt Clinic, general surgery is a key specialty. Our surgical procedures are performed by experienced physicians who have trained and practiced in prestigious clinics across Europe, the United States, and Israel.
The physical characteristics of your aneurysm will help your vascular surgeon determine whether endovascular treatment is right for you. In abdominal aortic aneurysms (AAA), eligibility depends on favorable positioning and a relatively straight aortic anatomy. The arteries also need to be wide enough to allow the stent-graft to pass safely and reach the targeted area, and the device must be able to conform to the shape of your aorta.
Endovascular stent-grafting is not limited to the aorta; it can also be used to treat aneurysms in other arteries throughout the body. Your vascular surgeon will carefully assess your condition and let you know if this technique is a suitable option for your treatment.
Request an appointment
Articles
Medical Services VenArt Clinic
Medical Procedures
Laparoscopic Interventions
Classic Surgical Interventions
Conditions Treated
Abdominal Conditions
- Gallbladder Disease
- Tumors of the Stomach, Liver, Pancreas
- Intestinal Pathologies
Pelvic and Perineal Conditions
Other Conditions Treated
- Thyroid
- Abdominal Lymphadenectomies
- Esophageal Tumors
Are There Risks of Complications?
If you have chronic kidney failure, the contrast material used during imaging can pose a risk, as it may further affect kidney function. Additionally, if your aneurysm has a complex shape, is associated with occlusive arterial disease, or if you have previously undergone AAA repair, the risks of the procedure may be higher. However, many of these risks can be anticipated and managed during the procedure—especially in cases where conventional surgery would carry even greater danger.
Your vascular surgeon will evaluate your overall health and specific condition in detail. Together, you will discuss the potential risks and benefits so the best and safest treatment option can be selected for you.
How Is the Endovascular Stent-Graft Process?
Before the procedure begins, you will be given sedation and either regional or general anesthesia, depending on your specific needs. The skin at the entry site—typically in the groin area—will be carefully cleaned and disinfected to reduce the risk of infection. A small incision will then be made over the femoral artery, through which a guidewire is inserted and advanced toward the aneurysm.
Because the walls of arteries do not contain nerve endings, you will not feel the catheter moving inside your blood vessels. You may, however, feel a gentle pulling sensation during the guidewire’s insertion.
With the help of advanced imaging for precise guidance, your vascular surgeon will insert a catheter over the guidewire and position the stent-graft exactly where it is needed. An angiogram is performed during this step to confirm proper placement. At that moment, you may feel a warm sensation due to the contrast material. Then, a compressed version of the graft is delivered through a larger tube called a sheath.
Once the graft reaches the correct location, the sheath is carefully withdrawn, allowing the graft to expand and seal firmly against the arterial wall. In many cases, additional components are placed through small incisions on both sides of the groin to support the arteries supplying blood to both legs.
What Can I Expect After Stent-Graft Implantation?
You will typically stay in the hospital for 2 to 3 days. On the first day after the procedure, you will be able to eat and begin walking. Once you return home, you should not drive until your doctor confirms it is safe. You may gently sponge around the incision areas, but it’s important to keep the groin incision sites dry until they are fully healed. Most patients are advised to avoid lifting anything heavier than a few pounds for up to six weeks.
Before discharge, your doctor will provide detailed instructions for your recovery. At your first follow-up visit, your doctor will check how your incisions are healing and assess your overall condition. In the first few months, you will undergo an imaging exam to ensure the stent is functioning as expected. Around the one-year mark, another imaging test will measure the aneurysm and compare its size over time. If any concerns arise, your doctor may recommend more frequent imaging to monitor the situation closely.
Are There Any Post-Surgical Complications?
Like any medical procedure, endovascular stent-grafting can have potential complications. Some possible issues include:
- Endoleaks, which occur when blood leaks around or through the graft
- Infections at the graft site
- Graft migration, where the stent shifts out of place
- Fracture of the graft structure
- Blockage of blood flow through the graft
In some cases, you may experience a low-grade fever and increased white blood cell count, which can last from 2 to 10 days. These symptoms are typically managed with medications such as aspirin and ibuprofen.
More serious, though rare, complications include:
- rupture of the artery
- kidney damage
- paralysis
- interruption of blood flow to the abdomen or lower body, which can be life-threatening.
Additionally, leaks between graft components may allow blood to flow back into the aneurysm—this is another form of endoleak. These can occur even years after the procedure and may become dangerous if the aneurysm begins to enlarge again.
Because of these risks, your doctor will recommend regular CT scans for life. Ongoing imaging helps detect any issues early, so they can be treated before becoming serious or potentially fatal.













